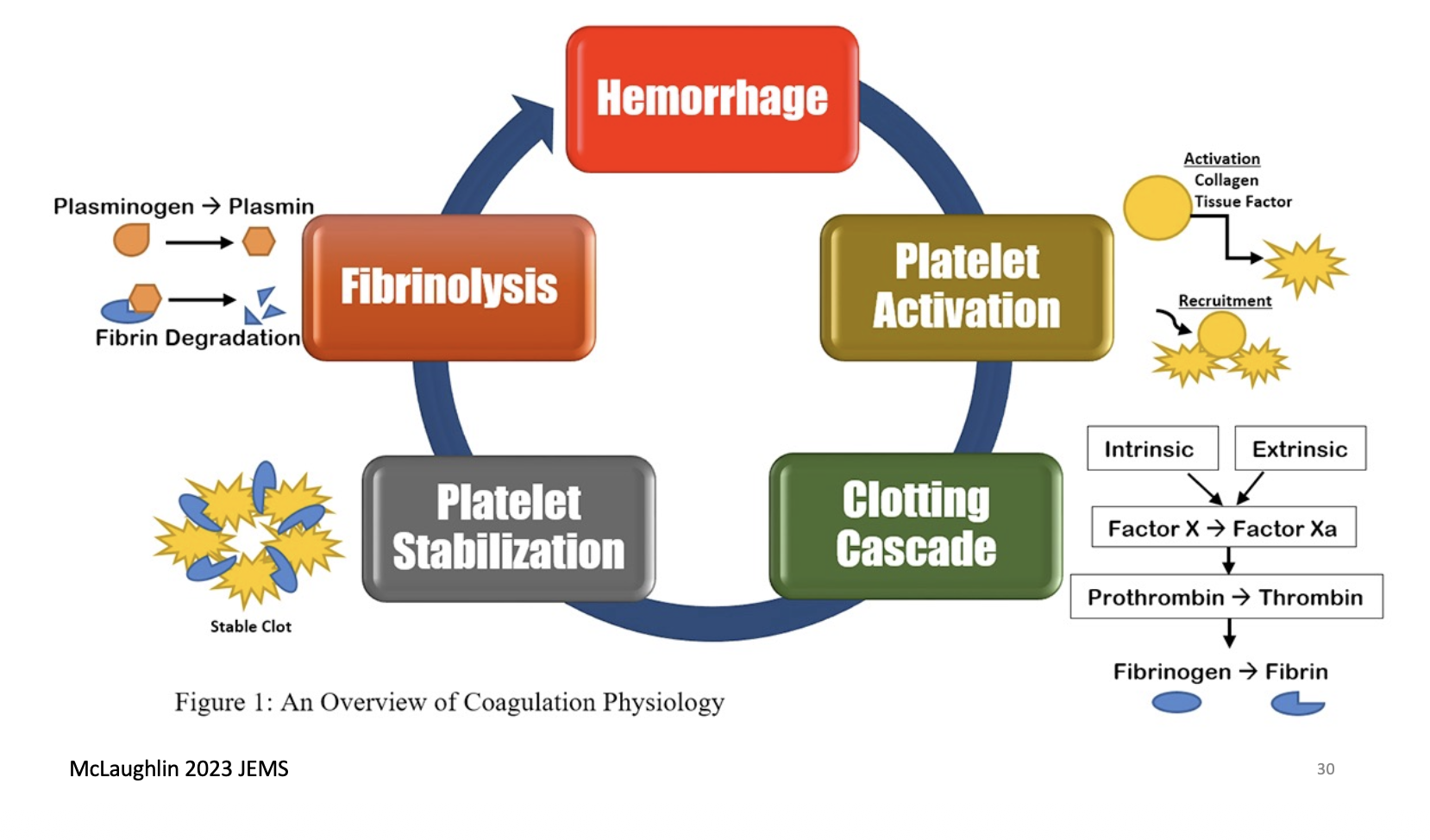
Coagulation is a process that results in Fibrin being laid down to cement a platelet clot in place. It is like glue and supports it while healing takes place. The main component is the coagulation cascade, a series of protein interactions that result in the laying down of fibrin,
The coagulation cascade can be intimidating and hard to remember because a lot of the factors are named by number. It is okay becasue there are plant of mnenomics to help.
| Factor | Name | Type of Molecule | Source | Pathways |
|---|---|---|---|---|
| I | Fibrinogen | Plasma protein | Liver | |
| II | Prothrombin | Plasma protein | Liver (vit K dependant) | |
| III | Tissue Thromboplastin or TF | Lipoprotein mixture | Damaged cells and pits | |
| V | Proaccelerin | Plasma protein | Liver, platelets | |
| VII | proconvertin | Plasma protein | Liver (vit K dependant) | |
| VIII | Antihaemolytic factor A | Plasma protein | Platelets, endothelium | |
| IX | Antihaemolytic factor B | Plasma protein | Liver (vit K dependant) | |
| X | Stuart-power factor | Protein | Liver (vit K dependant) | |
| XI | Antihaemolyic factor C | Plasma protein | Liver | |
| XII | Hageman factor | Plasma protein | Liver | |
| XIII | Fibrin-stabilising factor | Plasma protein | ||
Coagulation cascade parts
There are 3 main parts of the coagulation cascade, 1. the intrinsic pathway 2. the extrinsic pathway, and 3, the common pathway. Both the intrinsic and extrinsic pathways both lead to the common pathway and the common pathway leads to fibrin being laid down.
Extrinsic pathway 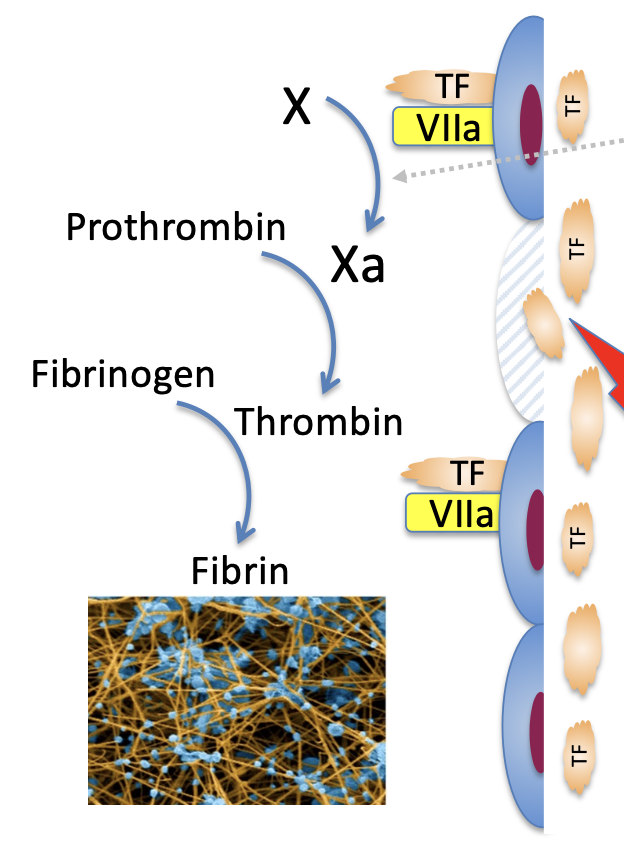
THe Extrinsic pathway is important to initate coagulation after endothelial damage.
How it works
This is called the extrinsic pathway because it needs Tissue factor (factor III, tissue thromboplastin) to get started, which is not included in the blood and is therefore extrinsic to it. Tissue factor binds to factor VII converting it to factor VIIa where both TF and FVII form a complex which acts directly to turn Factor X into Factor Xa, thereby starting the common pathway.
Testing
It is measured in the laboratory by the prothrombin time test (PT)
Intrinsic pathway 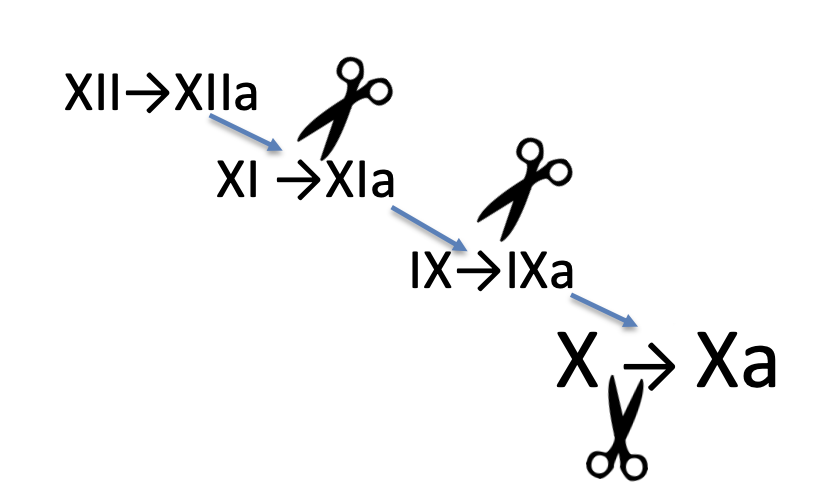
This has a few more bit to it but is still understandable. It is activated by negative charge so activation can be carried out by kaolin or silica. It is called the intrinsic pathway because everything needed for coagulation to occur is within the blood already.
How it works
Factor 12 (XII) is cleaved into factor 12a (XIIa) Factor 12a cleaved factor 11 (XI) to 11a (XIa) Factor 11a cleaves factor 9 (IX) to 9a (IXa) Factor 9a finally cleaves Factor X to Factor Xa
So basically 12-11-9-10
Testing
This is tested with the activated partial thromboplastin time (APTT)
Common pathway
The common pathway that the other 2 lead to is as follows:
Factor X is cleaved to factor Xa, which cleaves prothrombin to thrombin which directly turns fibrinogen into insoluble fibrin cementing the platelet mass in place.
Other bits and bobs
Cofactors
There are 2 other cofactors that speed up this reaction.
Factor V (when activated by being cleaved to Va) speeds up Factor X cleaving prothrombin to thrombin. I remember it by: 5 is half of 10 so it helps 10 half prothrombin
Factor VIII speeds up Factor IX cleaving Factor X to Xa, So really 12 → 11 → 8 & 9 → 10.
Membranes
All of this happens on membranes. Fibrin is a worse then useless cement if its just being made in the blood. It is best made on the actual endothelium and Platelets themselves because that is where its needed.
All coagulation needs 1. a phospholipid membrane, and 2. Ca2+ ion, to clot. (this is relevant when we try to do tests)
Fibrin (you can click on the images to make them bigger)
Now the structure and processes of fibrinogen and fibrin will be explained.
I think to understand it you really need to see it so i will include the pictures
Fibrinogen and fibrin structure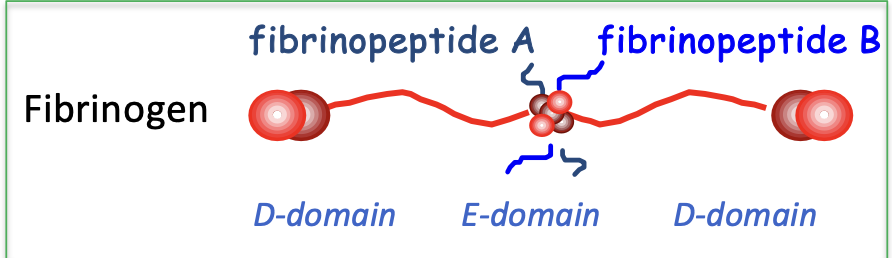
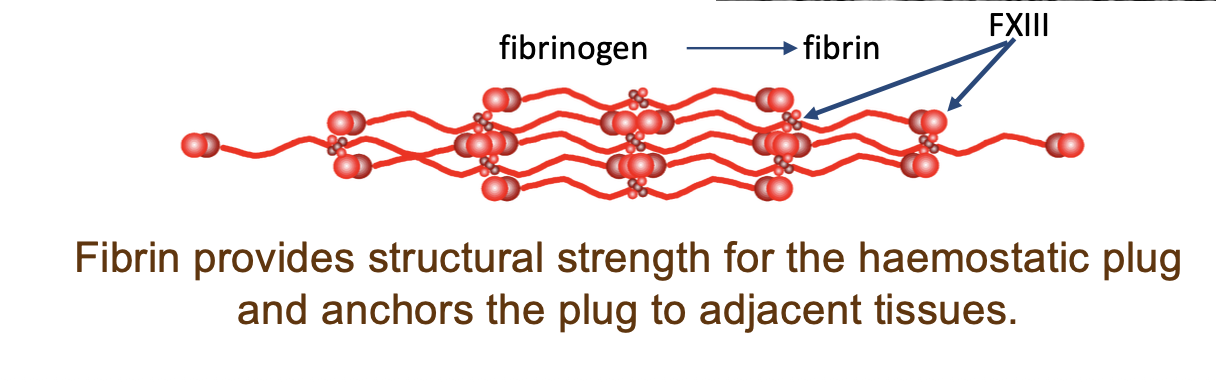
Fibrinogen is like a barbell looking thing and when it is turned to fibrin other fibrin molecules bind to it so it forms strings.
For fibrinogen to be turned into fibrin the A and B fibrinopeptides need to be cleaved off.
Fibrin cross linking and degradation 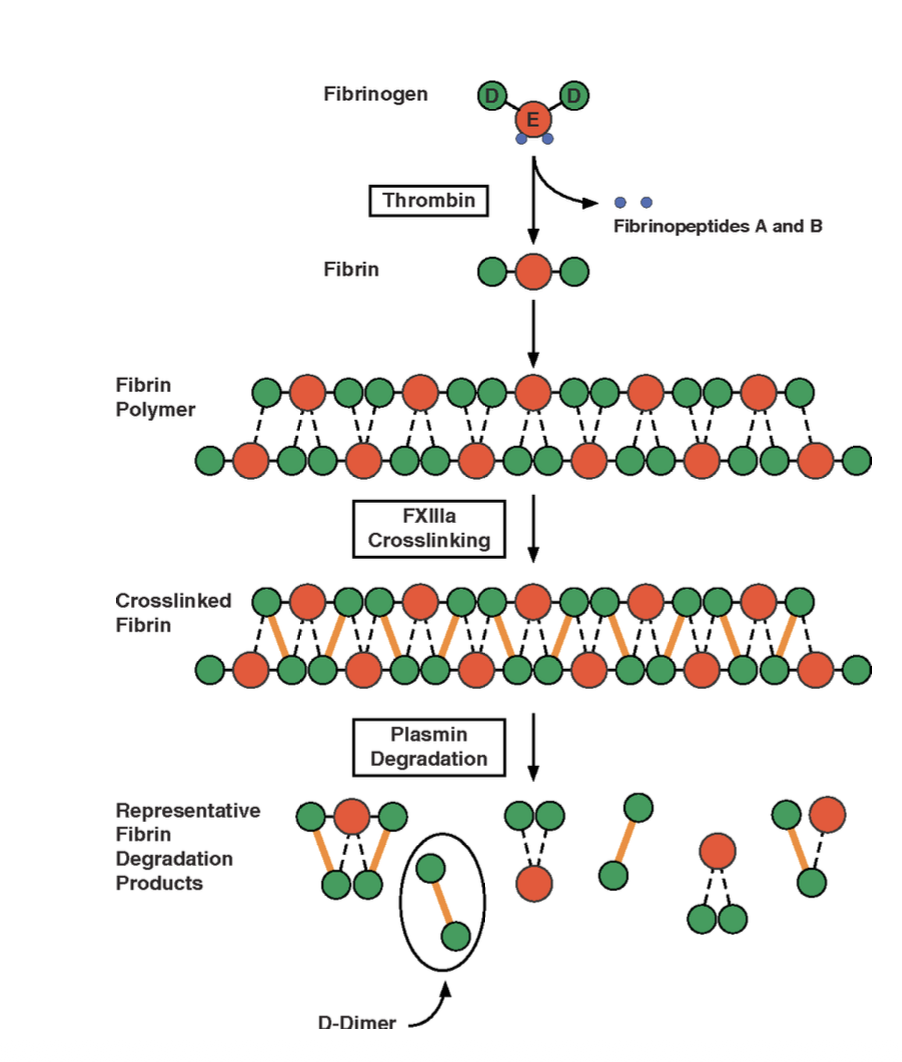
for fibrin to be strong it needs to be crosslinked. For it to be crosslinked FXIII needs to be present as it is involved in crosslinking.
Plasmin
The fibrin cement is constantly being degraded and dissolved from the point of its creation by plasmin, which also exists in the blood. If we didnt have this then we would be nothing but clot.
As Fibrin degrades come products are produced. One of these are D-Dimers which we can measure in the lab to assess if there is clot formation.
Sources of the factors
Basically everything here is made in the liver. Therefore liver problems will result in haemostatic problems.
Made in the liver:
- fibrinogen
- FII (prothrombin)
- FVII
- FIX
- FX
- FV
- FIX
- FXII
Factor VIII is not made in the liver however. It is made in the liver endothelium.
Vitamin K 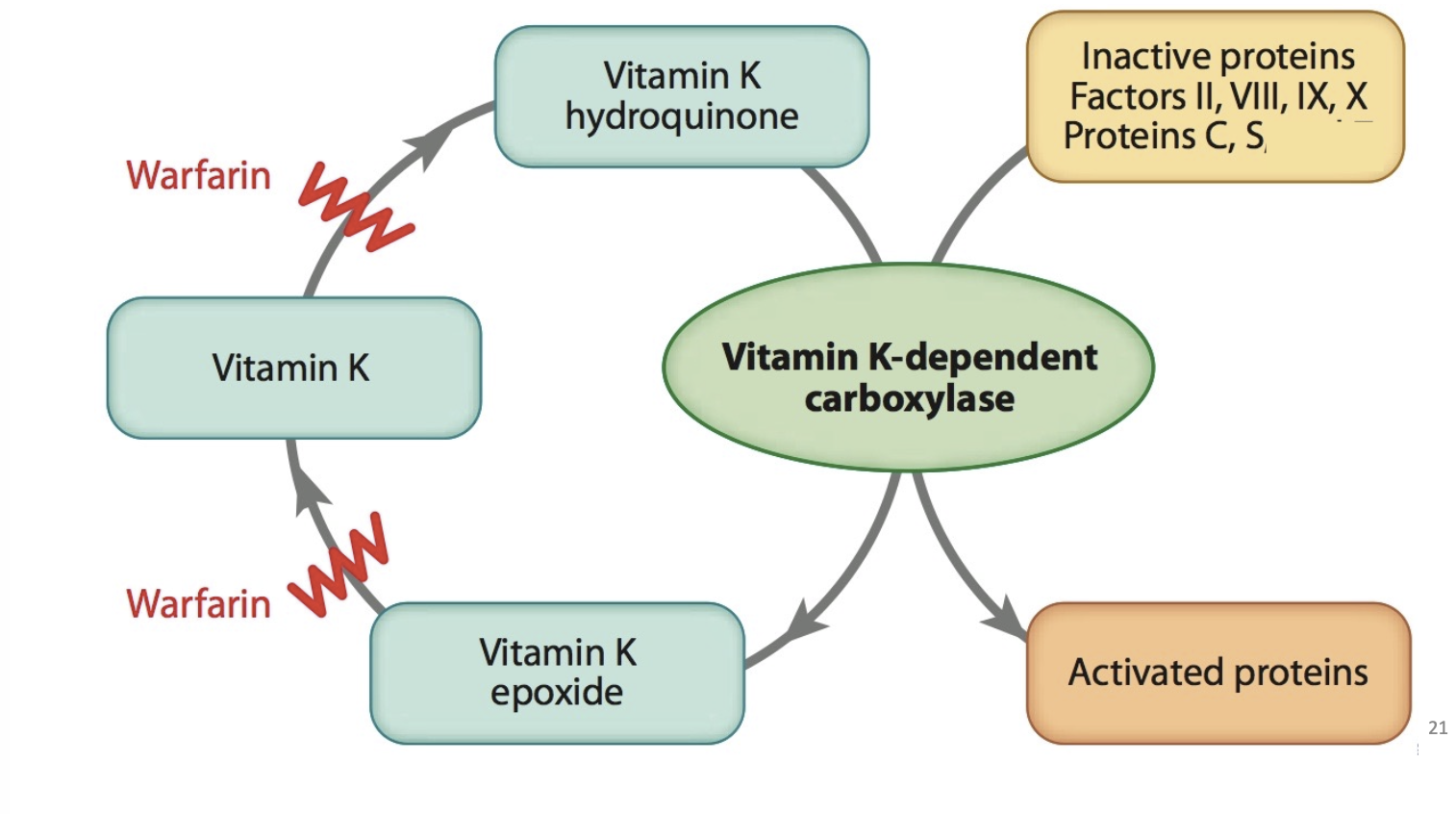 (koagulation)
(koagulation)
Factores 10, 9, 7, 2 (prothrombin), all need vitamin K for post translational modification ot make them functional. If you inhibit this they cannot stop bleeding or form clots.
Warfarin (coumarin derivative) inhibits Vitamin K regeneration is used to lower risk of stroke and other embolic pathologies.
Protein S and C also need Vit K to be produced
Inhibitors
We need inhibitors of coagulation or it would never stop,
Antithrombin bind irreversably to factors 11a, 9a, 10a, 2a and thereby inhibits them.
Protein S and C also inhibit factors 8a and 5a and inhibits them too.
Fibrin degradation
Plasmin eats away at fibrin clots. It comes from plasminogen. it is eventually inhibited by plasmin inhibitors.
tPA exists on healthy endothelial cells and both cleaves plasminogen to plasmin thereby clears fibrin from healthy endothelial cells
Synthetic tPA is injected into stroke and heart attack patients