Why do we have the cardiovascular system?
The cardiovascular system allows the blood to do its part”
- Providing oxygen and nutrients to the tissues of the body
- To remove unwanted by products of metabolism. CO2 and H+ ions
- and to transport all of these by bulk flow and at enough speed.
The circuits of the cardiovascular system
The structure of the heart is that it is 2 pumps, the right and left sides. these correspond to the pulmonary (right) and systemic (left) circuits.
Pulmonary Circuit
The pulmonary circuit allows the blood to exchange its carbon dioxide for oxygen and the systemic circuit allows it to go to everywhere it needs to go in the body as well as pick up and drop off contents. We have different circulations for this because it enables the lungs to be perfused without competing with organs allowing adequate oxygenation. It also allows the lungs to be a relatively low energy circuit with little work needed to perfuse it (the relative decrease in size compared to left heart.)
Systemic circuit
The orientation of this is so that most regions and organs are in parallel so that flow through one does not impede flow through another. There are however nuances to this.
Vasculature pressure changes 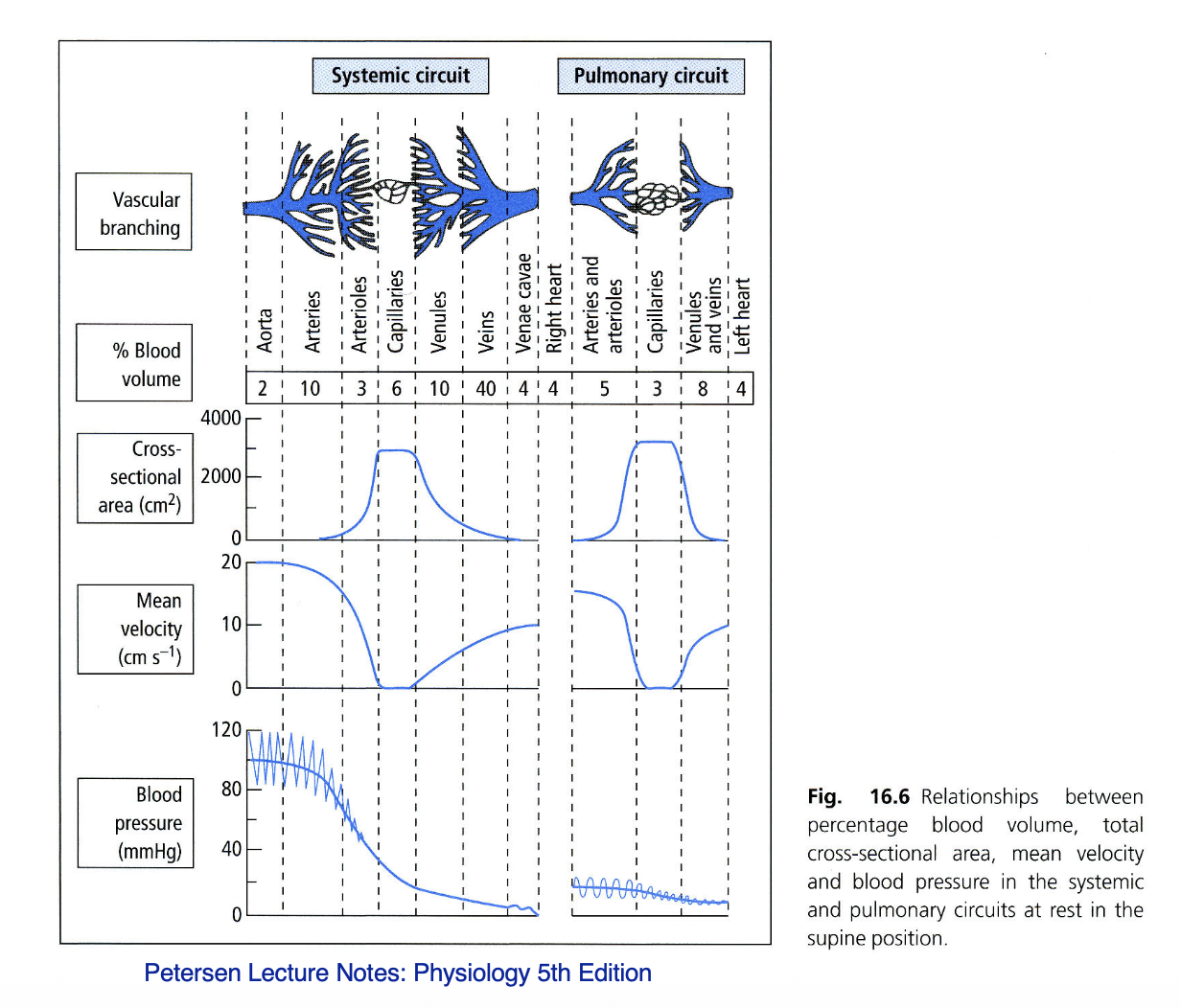
The order of vasculature in general is:
- Aorta
- Arteries
- Arterioles
- Capillaries
- Venules
- Veins
- Venae cavae
As it goes through each section the speed, pressure of blood changes with respect to the massive change in cross sectional area. This is because cross sectional area is by far the largest determinant of resistance in tubes and pipes. as the aorta moves to the capillaries you see a exponential increase in cross sectional area and then inverse exponential decrease in cross sectional area to the venae cavae. this corresponds with decrease and increase in speed but an overall decrease in pressure as there is nothing to drive pressure in the capillaries.
If you look at image closely you also see a great portion of the blood in veins and venules, this is because they act as capacitance vessels and store blood if you lose any.
Blood pressure equations
The job of the heart is to maintain a pressure gradient in the pulmonary and systemic circuits to allow the blood flow and do its job. The job of the blood is transport stuff to tissues and away from tissues. To do this it needs to move and enough of it needs to be moving to deliver the right amount of resources to meet requirements of the tissues.
There are a few equations that we can use to figure out what the blood pressure gradient is, so we can figure out enough blood if moving to properly deliver and take away,
These equations are:
Where CO can be calculated by
MABP = mean arterial blood pressure C0 = Cardiac output TPR = Total peripheral resistance HR = Heart rate SV= Stroke volume
Explanation
We need to keep MABP above a set amount of blood wont have enough impetus to go to all the tissues we need. We also cannot have it too high or we suffer from disease and damage.
MABP is made of 2 components, The cardiac output which is a measure of blood flow from the heart per second, and TPR, total peripheral resistance, which is a measure of the amount of resistance from the systemic circuit (we don’t worry much about the pulmonary circuit in this bit of physiology).
We can can calculate Cardiac output with the stroke volume, which is the amount of blood pumped per stroke, and the amount of strokes per second (heart rate) to give amount of blood per second.
So what?
The body has a mandate to keep blood pressure in the range to deliver adequate resources whatever the condition without causing damage and can regulate TPR, Heart Rate and Stroke Volume to keep MABP in range.
How does it do this?
Baroreceptors in the carotids send signals to the CNS constantly reporting what current blood pressure is. If it is high or low the body can react accordingly:
Heart rate
Stroke volume
Total peripheral resistance
Frank-Starling Law
The frank starling law is a large component of how the stroke volume changes. It is basically the idea that as there is more flow through the systemic circuit then the right side will fill up faster and generally more inflating the heart with more volume for a larger stroke.
In haemorrhage (Haemorrhage case)
If there is loss of blood there is less pressure as this lessens TPR. Your body will try and compensate in a few ways. But with enough loss this is not enough and there is persistent hypotension and shock, which can lead to death.
Compensation mechanisms
Immediate: Baroreceptor reflex
Your baroreceptors will trigger hr to increase, sv to increase and tpr to increase all leading to elevated to MABP
Intermediate: Autotransfusion/ starlings equilibrium
To under stand this you need to understand the Starling equilibrium. This describes the phenomenon of the push and pull of volume in and out of the blood. The blood has higher osmolarity and always attracts water to it. But it also has higher hydrostatic pressure. These culminate in a scale that balances itself in the end. On the higher pressure arterial side of the systemic circuit there is net flow outward due to higher pressures. Then on the lower pressure venous side of the circuit, there is net flow inward.
When there is significant volume drop from something like haemorrhage, on both sides arterial and venous sides of circuit there will be net volume inflow slowly propping up the blood volume.
Long term: Volume replacement
Over time your body will try and replace the volume lost with increase thirst, decreased renal loss from ADH and reduced renal perfusion. In the end you will have blood loss anaemia over death, but over tiem your body will make more RBCs.
Nuances to this physiology
if you are hot your body will send more blood to the skin, to lose heat. This drops your TPR and so your heart will pump a lot harder to compensate
Shock
Shock is what happens when you dont have adequate perfusion. This can be hypovolaemic (not enough blood), Distributive shock (where your blood vessel dilate and cause prolonged massive tpr reduction) and cardiogenic (heart failure).
This will be covered more in the future.