RAAS (context)
This is to give context on the associated drug system:
The Renin-Aldosterone-Angiotensin-System is involved in body regulation of water and salts.
The system is started with the release of renin from the kidney from juxtaglomerular cells in response to sympathetic stimulation, low blood pressure in kidneys, and low Na+ in distal tubule. These kick off the RAAS.
We then see a number of interactions occuring
Renin cleaves angiotensinogen produced by the liver to form angiotensin I
Angiotensin I is cleaved by ACE (Angiotensin converting enzyme) to form Angiotensin II a far more potent version. ACEs are often bound ot endothelial walls. The angiotensin II is can then bind to Angiotensin receptors I or II (AtI or AtII)
Angiotensin receptor 1 (AT1R) has a lot of potentially pathological effects such as Na+ reabsorption, vasoconstriction, and aldosterone release and in general is profibrotic, apoptotic, cell proliferative which are all bad things. Angiotensin receptor 2 (AT2R) leads to positive effects, such as antiproliferative, antifibrosis, and vasodilation
- Angiotensin receptors generally directly and indirectly lead to:
- Na+ and fluid retention
- increase in BP (vasoconstriction and fluid retention)
- Aldosterone secretion
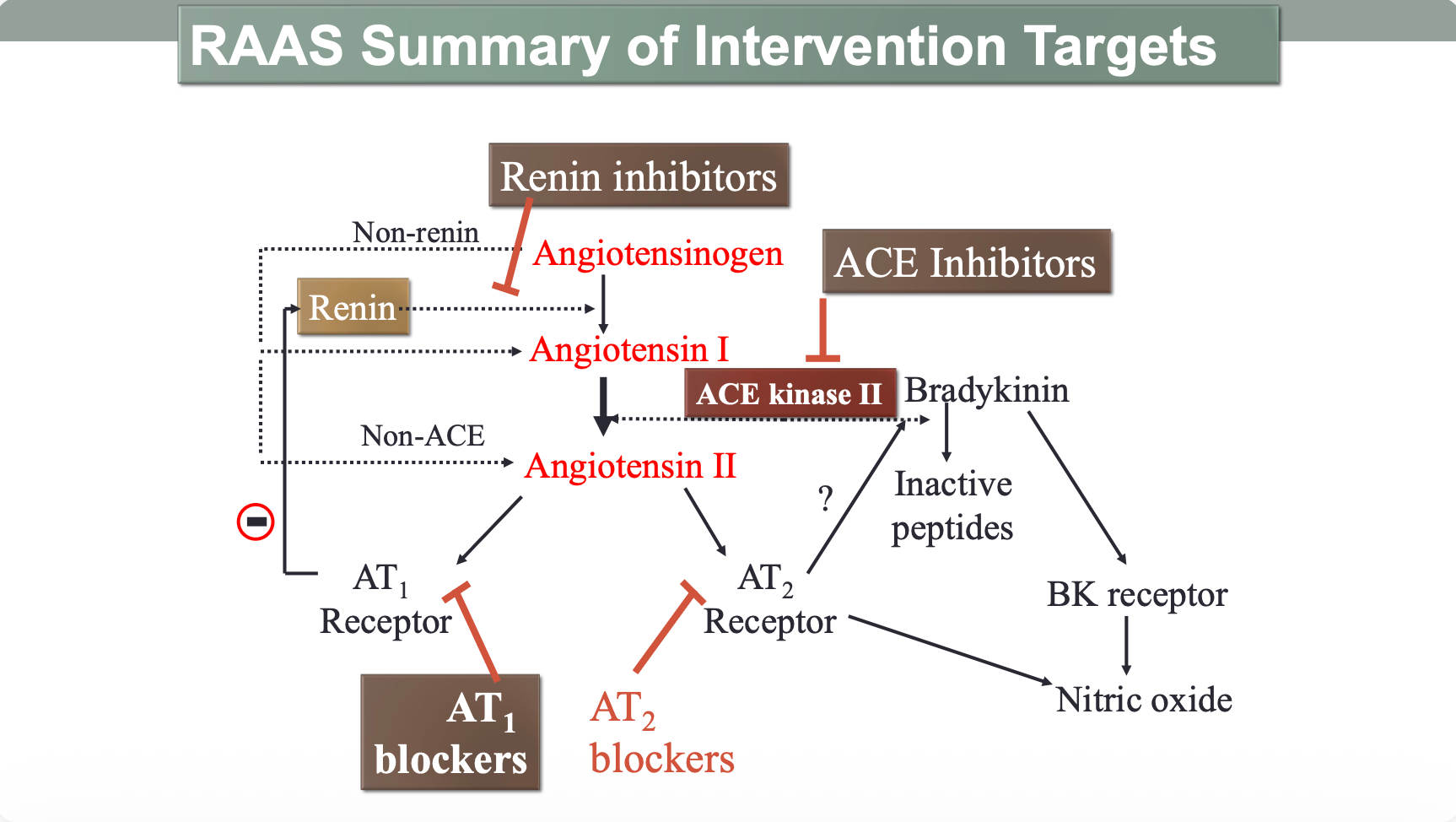
The RAAS can be modified at each of its points
- Reducing renin release (beta blockers and renin inhibitors)
- Reducing Ang II production (ACE inhibitors)
- Inhibiting At1 receptors (ARB inhibitors)
- Decreasing aldosterone mediated effects (Mineralcorticoid receptor inhibitor)
And these are all the ways the drugs will be covered.
(ACE also cleaves bradykinin to deactivate it so dry cough can occur in patients under ACE inhibitors)
The drugs
ACE inhibitors (‘pril)
These drugs inhibit free and fixed ACE
What does it do:
- Decreases levels of Ang II released
- Increases levels of bradykinin by stopping ACE from breaking it down
- reduces aldosterone production
- promote Na+ excretion and water excretion reducing plasma volume
- inhibit cardiac and vascular remodeling and fibrosis associated with CVD
Example:
Enalapril
For drug profile see link ^
Therapeutic uses
Primary and renovascular hypertension
-
Effects on cardiovascular system Produces arterial and venous dilatione reduces arterial and venous pressures
-
Effects on kidney Promotes natriuresis and diuresis Decreases Blood volume (lowers BP)
Effective in hyper-reninemic hypertension but still reduces BP in patients with low to normal renin levels (maybe due to bradykinin)
Additionally different ethnicities produce different levels on renin and will respond differently
Inhibition of Ang II production also crucial for proinflammatory and profibrotic effects of HTN
Chronic heart failure
reduced afterload reduced preload reduced sympathetic activation
and renal disease diabetes post MI stroke prophylaxis etc (MED3)
Adverse effects
- bradykinin related ADRs
- persistent dry cough and rarely angioedema
- initial hypotension
- rash
- disturbed sense of taste
- foetal abnormalites
- can lead to renal issues contraindicated in angioedema can cause swelling
ARBs (‘sartans)
selectively inhibits AT1R
- a lot of the same effects of ACE-Is have minus kinin accumulation and AT2R block
- may channel Ang II to AT2Rs to get increased positive effects
- additionally blocks Ang II no matter how its formed
- In theory is more beneficial than ACEs
Indications
- same for ACE inhibitors
- generally used when patient cannot tolerate an ACE-i due to ADR
- hypertension
- heart failure
- renal injury
Example
Candesartan Celixitil
Click link for drug profile