Objectives
Define the route of admin, site, and mechanism of the following commonly used drug classes and their specific examples
- ß₂ Agonists (vasodilators)
- SABAs: salbutamol
- LABAs: formoterol, salmeterol (Main focus now on the fast/ultrafast LABAs)
- Muscarinic antagonists (smooth muscle blockers)
- SAMAs: Ipratropium
- LAMAs: Tiotropium
- Leukotriene Antagonists: montelukast ()
- Biologics IL-5 monoclonal antibodies
Understand the limitations and adverse effects associated with each drug class; Identify the classes of drugs used in each step of asthma management.
Systems to control asthma
Drugs
ß2 -agonists
Mechanism
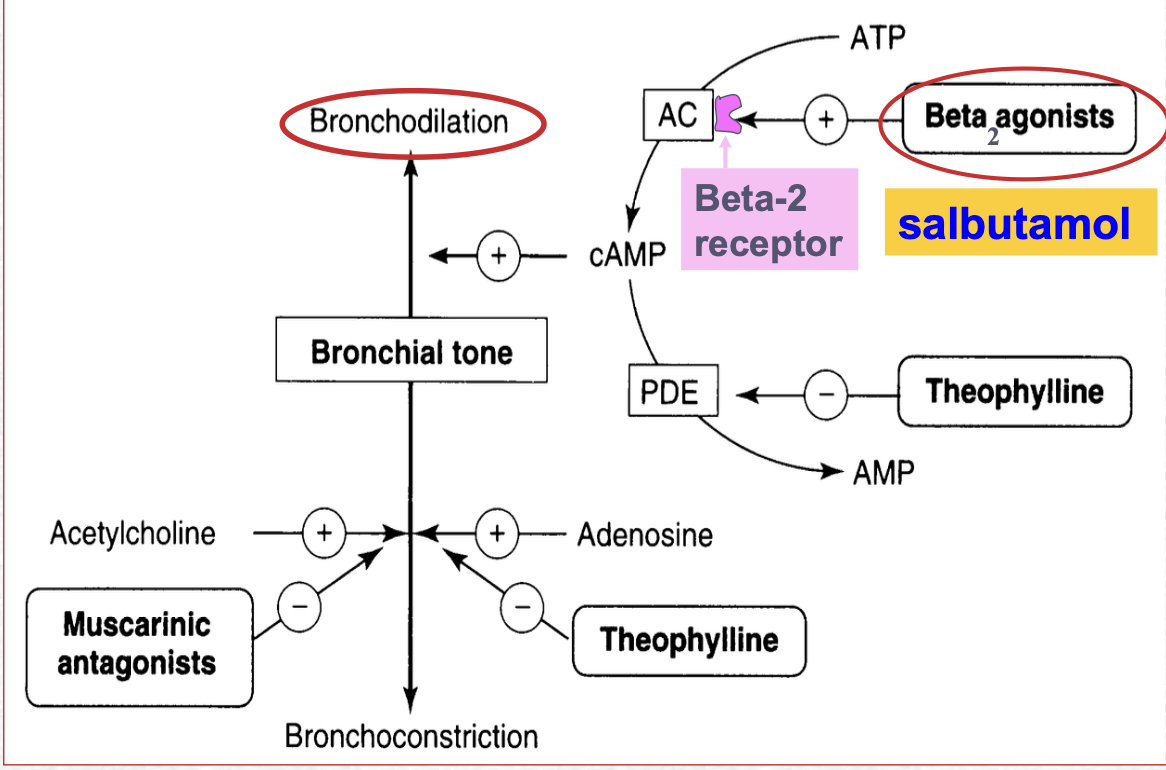
ß2 agonists activate the beta 2 receptor which promotes bronchodilation which drastically reduces airways resistance.
Specifically lecture states:
ß2 -adrenergic recpetor activation causes smooth muscular relaxation in response to endogenous catecholamines Effects of ß2 agonists on on airways smooth muscle:
- ß2 agonist activates cAMP activating PKA
- increase conductance od Ca2+ sensetive K+ channels in airways sm → hyperpolarisation and relaxation
- inhibits bronchial constriction Effects of ß2 agonist on epithelial cAMP
- increased ciliary beat frequency improves mucous and allergen clearance Issues with ß2 agonists are gene polymorphisms and “may underscore increased risk of exacerbations in COPD and asthma. (?)”
CONCOMITANT ß-BLOCKER USE IS DANGEROUS
Blocking of ß2 receptors are dangerous as they can aggrevate asthma DO NOT USE NON-SELECTIVE VERSIONS IN ASTHMA - propanolol, carvedilol Caution with ß1 selective ß-blockers - metaprolol, atenolol, bisoprolol
Drugs
SABAs:
Salbutamol
What lecture slides say about pharmacology of this drug:
- selective ß2 agonist and has ß2 selectivity 200 fold of ß1
- major role as rescue/reliever in asthma and COPD
- acute inhalation (from inhaler) to counteract bronchospasm
- treats symptoms 5-15 mins
- bronchosilatory effect lasts 2-5h
- preventing exercise induced asthma
- use on an as required basis (2nd tier approach)
- use lowest dose possible
- avoid regular fixed interval use - associated with adverse effects
- Causes ß2 recepotr downregualtion
What lecture slides say about ADRs of this drug:
At high doses with acute of short term dosing
- Tremor effecting peripheral skeletal muscle
- activation of skeletal muscle ß2 receptors
- Increased HR and force of contraction
- Can still effect heart ß2 receptors
- loss of selectivity on high doses
- dilates peripheral vessels → reflex tachy
- frequent use can produce tolerance
Brand names:
- ventolin accuhaler (blue wheel of cheese like)
- ventolin evohaler (looks like typical blue inhaler)
LABAs:
LABAs are not approved as a rescue inhaler. not reccomended for monotherapy
Salmeterol
This drug does not provide rapid relief and is rather for nocturnal asthma, exercise induced asthma, or an addon in COPD
The long acting bit comes from a long lipophilic side chain which resists degradation
What lecture slides say about pharmacology of this drug:
onset of action ~ 10-20 mins PEak effect ~1-2 hours Bronchodilatry effects ~12h dosing given regularly, twice daily
Formoterol*
Formoterol is a potent ß2 agonist (LABA) and is also fast acting. It replaces the need of SABAs
Symbicort is a combines budesonide-formoterol turbhaler
What lecture slides say about pharmacology of this drug:
Longer duration of action ~12 hrs Formoterol is fast acting with rapid (<1-3 mins) onset of action (Cmax ~6 mins) Combination with ICS –budesonide means that Symbicort is well tolerated with few issues.
Benefits of Fixed dose combination inhaler
Using LABA with steroids allows the steroid dose to be reduced LABAs adjunctive role ad a prophylactic better contol
LABA + ICS combination
- Symbicort (formoterol + budesonide)
- Seretide (fluicasone and salmeterol) complimentary medications!
Muscarinic receptor blockers
you want to specifically block the M3mAChR on the airway smooth muscle to block the contraction specifically. blocking the m1, m2, m4 receptors can lead to ADRS and may impact efficacy.
A note of paresympathetic NS role in COPD versus Asthma (and relation to muscarinic antagonists)
COPD major and reversible bronchoconstrictor component from the parasympathetic system, therefore SAMAs and LAMAs are advocated
Asthma the parasympathetic system plays a secondary role. However at night PS stimulation increases and may contribute to asthma effects so lamas are used as a nocturnal addon or at stage 4 and 5
Drugs
SAMAs
Ipratropium
What lecture slides say about pharmacology of this drug:
Inhalation route spirometric improvement peak onset - 30+ minutes durstion 3-5 hours given with ß2 agonist - additive effect indications most useful in COPD benefit in acute asthma emphysema
What lecture slides say about ADRS of this drug:
drug is not systematically absorbed but can produce ADRS
- dry mouth
- headache
- GI motility disorders
- cardiac events
- Urinary retention
- blurred vision ipratropium does not cross the Blood Brain Barrier
LAMAs
Tiotropium Bromide
What lecture slides say about pharmacology of this drug:
once daily LAMA for maintenance sparingly soluble in water; administered by dry powder inhalation aqueous solution (5mg) delivered via a spiriva respimat inhaler DRY powder (18mg) delivered by a breath actuated handihaler PKs: Peak spirometric improvement onset (30-60)
- maximum plasma concentrations observed 5-7 mins after inhalation with effective half life of 27-45 hrs
- majority of delivered dose is deposited in the GI tract where it is degraded and to a lesser extent int he lonf where 17% may become systemically bioavailible
PKs: Peak spirometric improvement onset