What is is inflammatory bowel 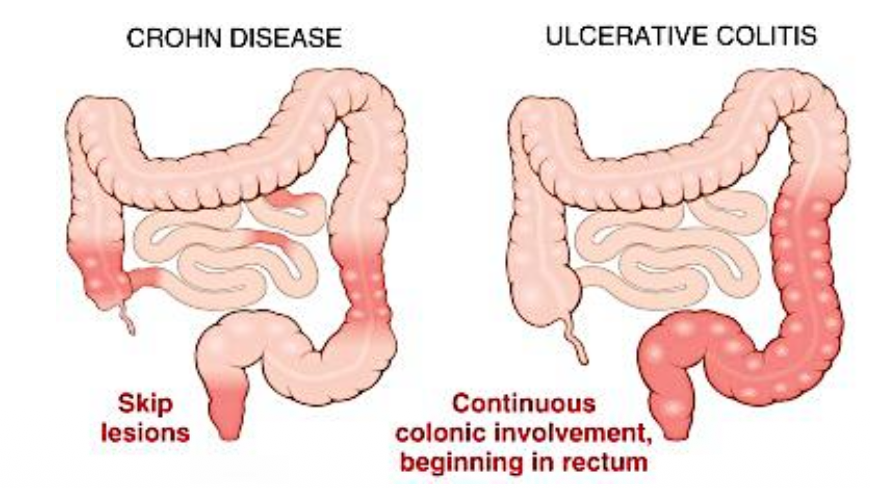
Inflammatory bowel is a chronic inflammatory condiation with acute exacerbations. It affects teens and people in their early 20 usually. 2 morphological type of the disease exists. Ulcerative colitis and Crohn dissease. They affect different parts of the bowel
Pathological profile.
Proposed pathogenesis
The proposed mechanism is complex with gneetics, intestinal microbiota, defects in gut epithelium and patients immune system all being implicated. These are all implicated,
- Defects in intestinal epithelial barrier leading to increased uptake of luminal bacteria
- activation of macrophages and production of cytokines and t helper cells
- Genes such as NOD2
Crohn disease
Crohn disease can occur in anywhere in the gut from mouth to anus, however the most common sites on involvement are the terminal ileum, ileocecal valve and cacum. The disease usually occues in a patchy way with skip lesions. Inflammation is transmural where gut wall is thick swollena nd rubbery. If suffered at length stricture formation can occur.
Gross morphology
inflammation leads to the development of deep linear fissures or knife like ulcers. The appearance of the ulcers are islands of uninvolved bulging mucosa leads to cobblestone appearance. Extensive inflammation leads to fat wrapping from the mesentery to around the serosa
Microscopic morpholgoy
There is transmural inflammation with high numbers of neutrophils inside the mucosal crypts (crypt abcesses) (this is not specific to ulcerative colitis)
Granulomas are a hallmark of crohn disease (these are non caseating and are causes by Th1 cells)
You can also see the fissure ulcers in the microscopic slides
Complications
Extensive small intestinal disease can lead to malabsorption. The walls are affected by fissure ulcers which can lead to perforation and abscess formation. Fissure extension through a wall and involvement of adjacent bowel loop can create a fistula between the 2 organs. Opening of. a sinus to the surface of the skin leads to sinus formation
Ulcerative colitis
This involves the rectum and then can extend to the entire colon (but not always). Colonic involvement in continuous with no skip lesions the small intestine is not usually involved but mild mucosal inflammation may extend to the terminal ileum (backwash ileitis)
Inflammation is limited to the mucosa and the superficial submucosa
Morphology
We see ulcerated mucosa with islands of regenerating and uninvolved mucosa projecting into the luman forming pseudo-polyps. These are a hallmark. There can also be crypt abscesses.
Complication
Though inflammation is limited to the mucosa and submucosa inflammatory mediatiors can reach the muscularis propria and inhibit neuromuscular function, leading to colonic distention and toxic megacolon. this can perforate and lead to septicaemia and death. total colectomy is performed in this case
Clinical
Clinical presentation isL Crohns: most patients with crohn disease present wiht intermittent attacks of mild diarrhoea fever and abdominal pain. Few patients present with acute abdominal pain and bloody diarrhoea. There will be periods of disease with asymptomaticity.
Ulcerative colitis: Patients present with relapsing attcks od severe abdominal pain and bloody diahorrhea with stringy mucoid material. Symptoms may persist and even require colectomy when uncontrollable by medications
Extra intestinal menifestations
- Uvelitis
- migratory polyarthrirtis
- Sacroiliitis
- ankylosing spondylitis
- clubbing of the fingers
- Primary schlerosing cholangitis