Meningitis is inflammation of the meninges. There are many different causes of meningitis each with its own implications and complications.
CNS infections
Meningitis is a subset of CNS infections/inflammations. These are all life threatening with high morbidity and mortality. as the CNS is enclosed by a rigid and unyielding container (the skull) it is very vulnerable to increase in pressure. Increase in intracranial pressure pushes on the brainstem, which can depress respiratory and cardiac centres (stopping the heart? and lungs).
To avoid this quick recognition and response is crucial,
The differences in CNS infections are by the site and therefore tissue of infection, causative agent and the host response. They present as chronic or acute.
Some examples of CNS infections are:
- Meningitis (inflammation of the meninges) (This can be caused by infectious agents (bacteria, viruses, and fungi) and non infection agents like subarachnoid haemorrhage drug reactions trauma etc.)
- Encephalitis (Inflammation of the brain matter) (usually caused by viruses)
- Meningoencephalitis (Inflammation of both the meninges and the brain matter) (can be caused by viruses and parasites)
- Abscesses (where bacteria or fungi eats through the brain)
What is Meningitis?
As detailed in the equation above meningitis is inflammation of the meninges. This can be pathogenic, or it can be chemical or even physical, but we will focus on the pathogenic causes.
To better understand the complications and implication of this condition it is helpful to understand what the meninges are. The meninges are a set of 2 membranes covering the brain that work to line and protect the brain and spinal cord as well as circulate blood and CSF around them.
The 3 layers are 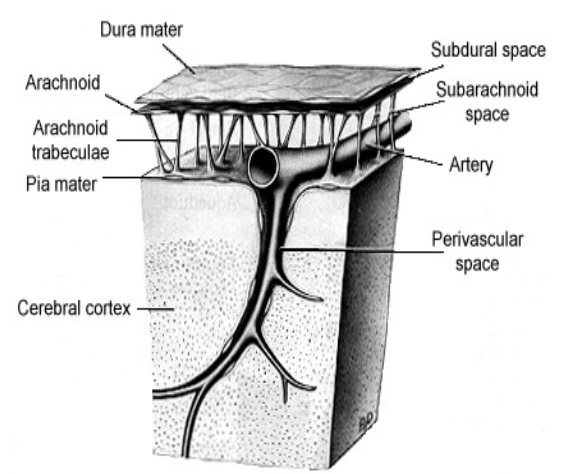
-
Dura mater: Dura mater means tough mother, and it acts as a tough protective layer foremost. it is the outermost layer.
-
Arachnoid This means spider like, referring to the spiderlike projections called the arachnoid trabeculae. These trabeculae hold the central arachnoid layer up away from the brain and spinal cord, creating a space called the subarachnoid space. In this space the Cerebrospinal fluid flows and vasculature runs.
-
Pia mater This is the “Delicate mother” and is the innermost layer
Sterility
The meninges and CSF are sterile in health and so any organism found in them is significant.
Classifications of Infectious Meningitis
The 3 types of infection in tne meninges are as follows:
Acute:
This is a purulent infection and bacterial in origin. We see bacteria and neutrophils in the CSF
Aseptic:
This is viral and is characterised by Lymphocytes in the CSf
Chronic (Granulatomous)
This can be bacterial or fungal. If bacterial it will be specifically TB, or syphilis. If fungal then it will be cryptococcus (which i think is only really a factor in AIDS sufferers).
Route of entry
The CNS tends to be a sterile place and so often there needs to be a way the infectious organism get there. The main ways are:
-
Haematogenous spread
This is where the pathogen travels in the blood to reach the brain. It is the most common and bacteria fungi and viruses all do it.
-
Direct inoculation
This is where something pierces the physical barriers that protect the CNS and serve as a way of entry for pathogens. This can be traumatic, or iatrogenic (neurosurgery, CSF shunts, lumbar puncture, etc)
-
Contiguous spread
This is where a local infection can spread into the brain. Most head infections have the potential do this.
-
PNS → CNS
Viruses like herpes can do this
Causative organisms
(This and the next bit is really flashcardable) Bolded is most deadly
Bacterial origin: If the meningitis is of bacterial origin then usually it is respiratory or traumatic/surgical:
- Respiratory: Neisseria meningitidis, streptococcus pneumoniae, haemophilius influenzae
- Trauma/surgery: S. aureus, S. epidermidis, streps, gram-negatives Viral origin: Viral meningitis is usually self limiting and rarely severe. (If there is no encephalitis)
- Enteroviruses, Herpes, Measles, Mumps, Influenza Fungal origin:
- Cryptococcus (Characteristically found in immunodeficient and HIV sufferers) Parasitic origin:
- Protozoa can lead to meningoenchephalitis (Naegleria fowleri, Toxoplasma)
Causative agents with age
very flashcardable. N. meningitidis (Meningococcal meningitis) is the most important cause 3 mths - 50 yrs
| Age/condition | Organism |
|---|---|
| Neonate (immature immune system) | E. coli, S, agalactae, S. epidermidis, listeria monocytogenes, HSV |
| <2mths (Colonised at birth) | E. Coli, S. agalactiae, L. monocytogenes |
| >2mths to 10 yrs (Immune system developing) | Haemophilius influenzae, Neisseria meningitidis, S. pneumoniae, Viruses |
| Adolescent | N. meningitidis, viruses |
| Adult | n. meningitidis, S. pneumoniae |
| Elderly/Immunocompromised | S. pneumoniae, l. monocytogenes, gram -ves |
| HIV/AIDS | Cryptococcus |
| Trauma/Iatrogenic | S. aureua, S. pyogenes, S. Pneumoniae, gram -ves (Pseudomonas) |
Clinical features
Signs and symptoms
- Fever (39-40 is acute bacterial)
- Neck stiffness
- photophobia
- neurological → headache, papilloedema, altered mental state, seizures
- Lethargy, vomiting, diarrohea, myalgia, arthralgia
- Cold, pale extremeties, mottled skin
- Sepsis and shock
- Rash
- Nonblanching (Doesnt go away with pressure) suggesting Disseminated Intravascular Coagulation (DIC)
Classic triad
The classic triad of meningitis is fever neck stiffness and headache but this is not always present 20-66% of cases and fever is the most common at 95% of cases.
Infants
In infants you must looks for generalised symptoms (lethargy, irritability, poor feeding), and high pitched cry and bulging fontanelle.
Rash
N. meningitidis has a characteristic rash which is not always present but is very suggestive. It is from septicaemia depletion of clotting factors in blood, Petechiae is small, purpuric is large and do a glass test to see if it blanches, this is bleeding into the skin
Kernig’s/Brudzinski’s signs 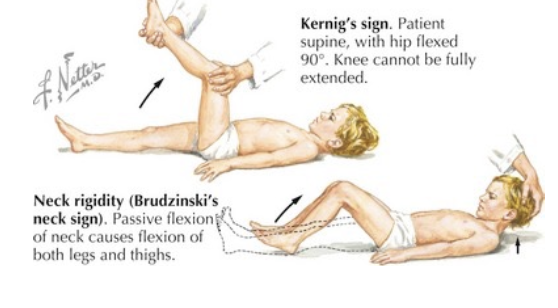
Kernigs and brudzinskis signs look for meningeal irritation. Low sensitivity though
Complications
- Death
- Amputation
- hearingloss/blindness
- Epilepsy, cerebral palsy
- Cognitive issues, developmental delay
The risk groups are
- Infants and elderly
- Adolescents (students)
- Immunosuppressed
- trauma or head infecctions
- CSF shunts or neurosurgery
- Asplenia (lack of spleen) (spleen is really important for clearing opsonised bacteria from blood)
- bacteraemia, fungaemia, viraemia
Diagnosis
Diagnosis performed by taking csf via a lumbar puncture ideally before antimicrobials are given.
CSF tests
Visibility
Normal CSF is watery clear, and colourless. Visible turbidity is cells in the CSf. green colour is pus and orange/yellow/pink is blood (haemorrhage).
WBC screen
Performing WBC screen can tell if its acute bacterial or viral Bacterial: WBC (neutrophils), protein up, glucose down Viral: Lymphocytes up, protein up
CSF gram stain
Gram staining of CSF can be affected by antimicrobials already administered.
Culturing
You can culture the CSf for bacteria and look for sensitivities to antimicrobials. Additionally you can culture the blood to see if there is any bacteraemia or septicaemia.
Bacteria and viruses
You can perform PCR which is a rapid test to identify the pathogen. it is not affecte dby prior antimicrobials and you can use small volumes of CSF which is good for neonates and children
Treatment
For acute bacterial meningitis use prompt empiric antimicrobials and untreated infections/delays relsult in significant preventable mortality and complications.
Empiric therapy
Prehospital treatment use IM ceftriaxone (or penicillin) Look at nz guidelines Empiric hospital treatment is IV ceftriaxone If Neisseria Meningitidis is suspected IV ceftriaxone should be administered and rifampicin for close contacts and carriage
H. influenzae: use IV ceftriaxone S. pneumoniae: use IV penicillin, or possibly empiric therpy shifts to IV Vancomysin and ceftriaxone as Penicillin resistance rises
In neonates: IV penicillin/cephalosporin with gentamycin (add ampicillin if you suspect listeria)
Other treatments
Steroids You may be able to use steroids to reduce inflammation but it isnt proven
Vaccinations There exists multiple vaccination options for some major causes of bacterial meningitis. These are reccomended for risk groups (students etc.)
S. pneumoniae has vaccinations for most common capsule types H. influenzae bas a b type vaccines N. meningitidis has A, C, Y, W vaccine and new B, vaccine that is now part of the schedule. Influenza vaccines