Cell injury
Cell injury can be caused by many things like: Hypoxia, Ischemia, Chemical agents, Physical agents, Infectious agents, Genetic abnormalities, Lack of substrates. and cells can either adapt to these changes or die.
Variation of injury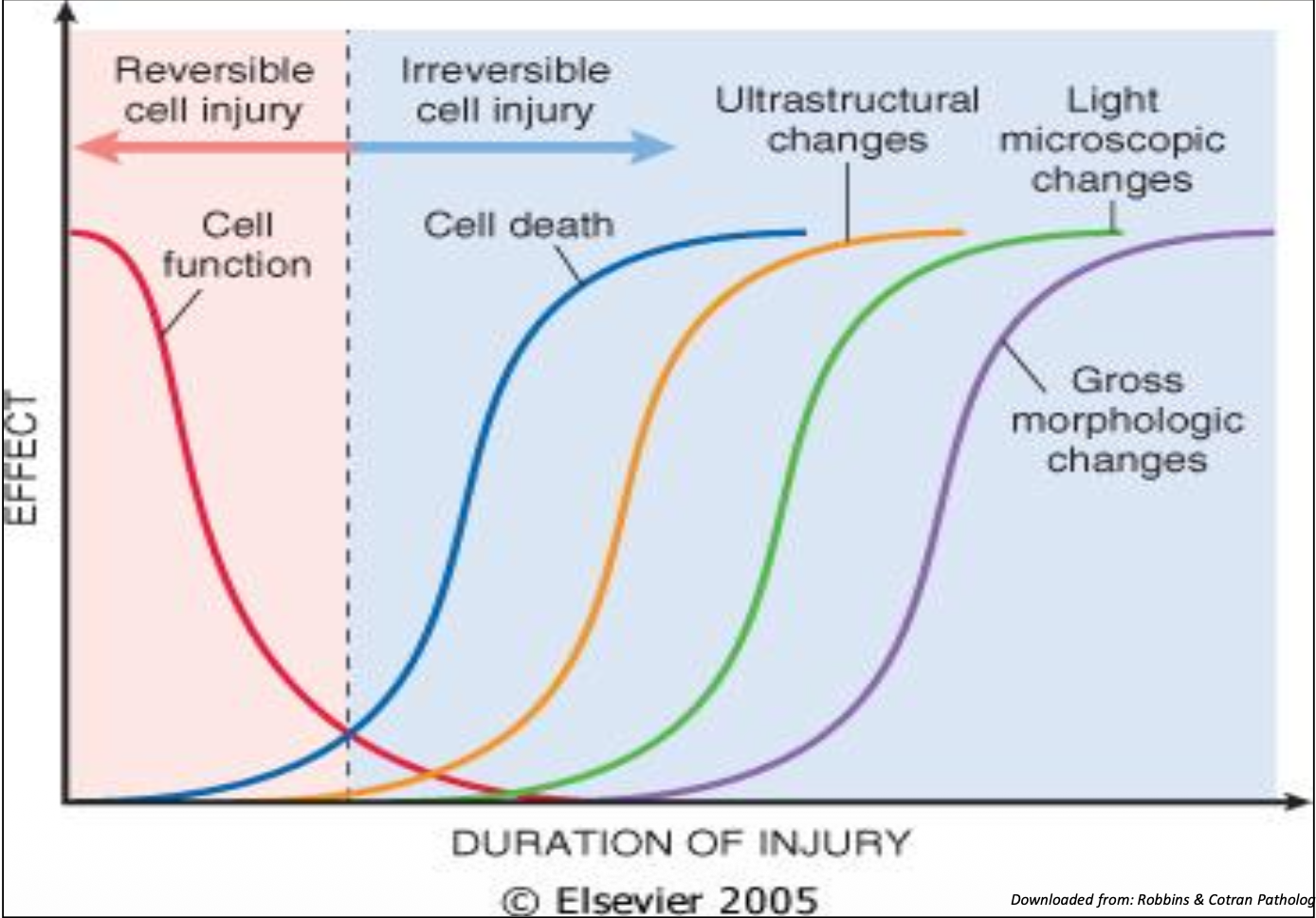
Cell injury can be reversible or irreversible depending on severity and duration of injurious insult. This graph sums this idea up nicely. The cell function is lost before you can actually observe signs of injury. Additionally the duration of the injury has a significant effect on the signs of injury.
Stepwise process of injury 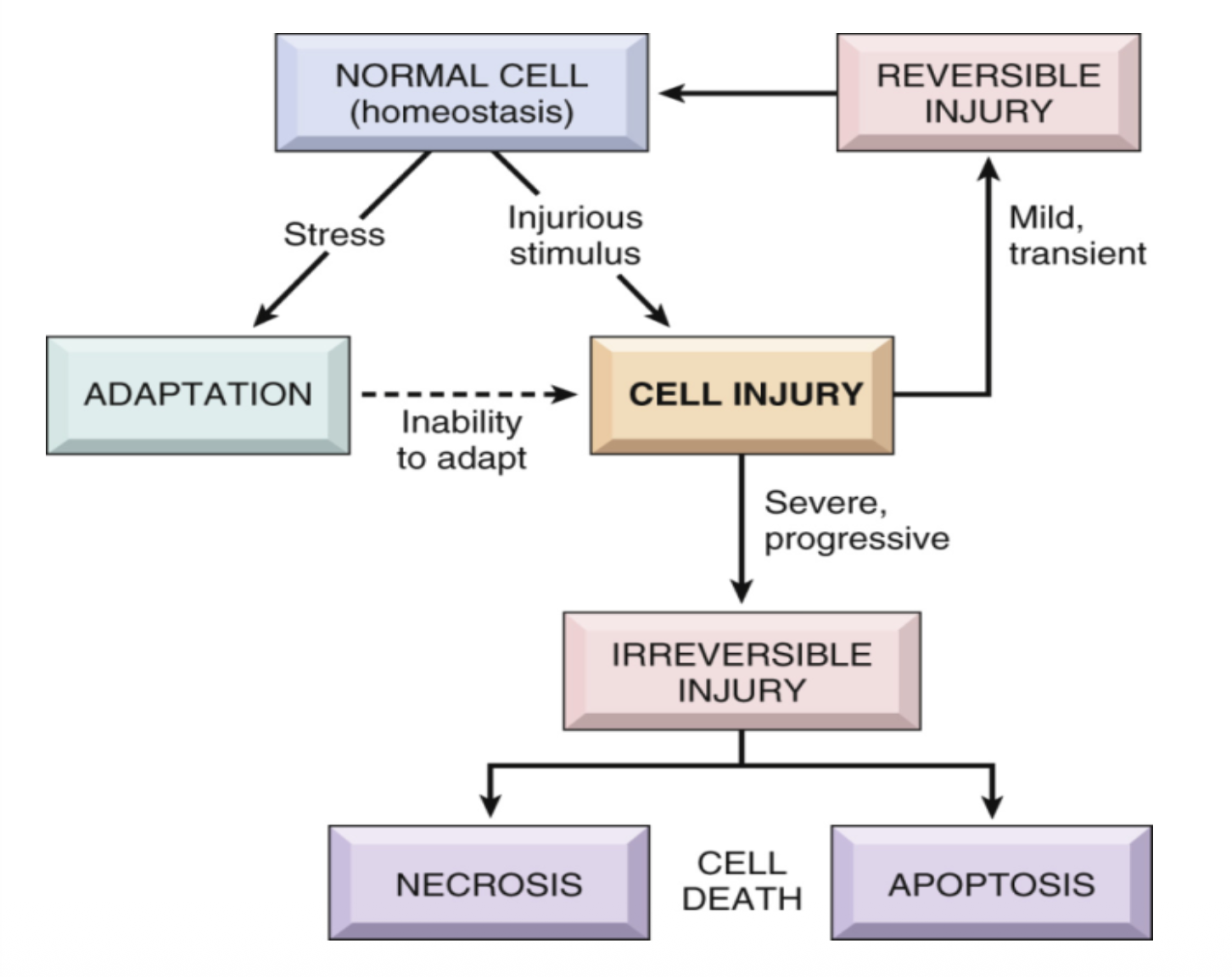
A normal cell upon exposure to an stressor or injurious stimulus will either adapt or be injured. If there is a failure to adapt to a stressor injury will result. Injury can be reversible, and the cell will return to normal state after the insult subsides. If it is severe and it doesnt fgo away necrosis and apoptosis will result. (explained later)
Hypoxia in specific
Hypoxia specifically can cause damage because energy obtained from oxidative metabolism needed to maintain the mechanisms of the cell will not be present in high enough concentrations (eg energy for pumps to do their things)
Cell injury signs (morphology)
On microscopy the injured cell can appear swollen and blebbed (with little bits starting to look like its coming away). Accumulations of waste and other substances may also appear in the cytosol.
Cell Adaptations
To an injury a cell can adapt. For example in the harsh conditions of a smokers lung the respiratory epithelia can metaplase into stratifies squamous epithelia. This mean more protection but no mucosal clearance with cilia. This is an example of metaplasia. There are 5? ways adaptions can occur: hyperplasia, hypertrophy, atrophy, metaplasia, dysplasia.
Hyperplasia
In hyperplasia cells multiply to better deal with the stress conditions. We see this in goitre as the cells sense not enough t3 being made and so therefore multiply to make more unfortunatly none will be made as there is usually a lack of iodine
Hypertrophy
This is where the cells enlargen themselves to better deal with stressors eg in high blood pressure an enlargened heart wall is seen as the cardiomyocytes swell in size to be able to pump harder
Atrophy
Atrophy is where a cell decreases in size either as failure to adapt paradoxically or as the current size isnt currently needed
Metaplasia
This occurs in tissues that need to change cell type to survive eg in smokers lung a transition from respiratory epithelia to simple stratified for protection.
Dysplasia
This is where malignancy develops by chance after a metaplasic shift eg rapidly dividing simple stratified epithelia develop into cancer as they are rapidly dividing and accumulate mutations more rapidly, reflecting their high rate of division.
Cell death
Cell death occurs normally or pathologically Normal death is called apoptosis
Many pathways to cause this: dna or protein damage, viral infection, outside influences etc
Occurs after enzyme cascade of proteolystic caspases which make apoptotic bodies Abnormal, unintended cell death is called necrosis This is where the cell cannot maintain its processes to stay alive, Messy, inflammatory and alarming raising molecules are released There are other mechanisms for cell death eg necroptosis pyroptosis ferroptosis etc) 3 stages of nucleus damage Pyknosis dark pinpoint Karyorrhexis fragmentation Karyolysis nothing
Healing
Healing starts with inflammation
Macrophages play a key role in healing through the removal and cleaning of necrotic tissue and release of TGF-b
Regeneration and scarring - 2 outcomes
Regeneration is possible where there is minimal damage
Scarring is for larger damage
Steps of healing by fibrosis in
-
Formation of new capillary vessels (angiogenesis)
-
Budding of new blood vessels from presexisting ones
-
Driven by Vasculatr endothelial growth factor, fibroblast growth factor, and angiopoetins
-
Formation of grandulation tissue
-
Fibroblasts migrate to the site of injurt and proliferate
-
They make ecm mainly collagen
-
TGFb id released from macrophages and are the main drivers of this
The mixture of new capillary vessels, fibroblasts, collagen, and remaining inflammatory cells all together make granulation tissue
-
Maturation and remodeling of the fibrous scar
-
Granulation tissue matures into a fibrous scar the fibroblasrs and blood vessels decrease and the collagen increases
-
Excess collagen is degraded by Matrix metalloproteinases
Factors influence the rate of repair
Wound infection
Diabetes
Nutritional status
Poor blood supply
Mechanical factors e.g. Too much movement
Foreign body in wound
Primary intention is easy relatively scar free tissue due to well opposed, close edges
Secondary intention is fat ugly and scarring
Some complications include rupture
Infection
Exuberant granulation tissue
Hypertrophic scar
Keloid
Bone fracture
Haemotoma
Big clot and bleeding
Granulation tissue forms
Soft callus
Bony matrix and some cartilage staryt forming
Hard callus
Ossification forms
Remodeling
Osteo clastic and blastic activity resorbs excess cellus
Complications:
Nonunion
Fibrous union