This touches on persistent pain and its effects, as well as pain in general
Patient understanding of pain
People often have no understanding of pain at 68%, People also often doubt the reality and impact of pain at 65%. The total costs of pain management in NZ are 15 billion in 2016 which is a lot of money, and 20% of the the NZ population experiences persistent pain.
Persistant pain
The effects of ongoing pain (important for exams)
Ongoing pain can being about
- Distrust in the medical system
- Feelings of invalidation
- Feelings of making it up
Persistent pain can influence how you act and how you feel about yourself
It can change how you are in society:
- Loss of employment
- Changes in role
- Limited social interactions
- Leading sense of burden
Pain terminology
What is Pain?
It is an unpleasant sensory and emotional experience associated with actual or potential tissue damage or describes in terms of equivalent damage
It is more than just physical experience as we see later (Panicaption is not pain)
Acute vs chronic pain (important for exams)
Acute pain is less than 6 months It usually has/is:
- recent onset and limited duration
- A waring sign of damger
- Facilitating healing through immobilistion (try not to move)
- Less complex psychological processing and social acceptance
Persistant pain (Persistent Somatic Symptoms is now the preferred umbrella term)
Persista\ent pain defined as pan longer then 6 months (kinda arbitrary timeframe)
- Pain persisting beyond expected helaing of injury
- Often no identifiable cause
- Complicated psychological processing and social acceptance
Acute pain to persistent pain
To understand a theory of how persistent pain develops it is helpful to understand the mechanisms of pain:
Pain mechanisms
Nociception
Nociception is the nervous response to sensory neurons sensing noxious stimuli. This is sent to the brain and eventually a experience results: pain.
Nociplastic
Nociplastic response is altered nociception. There is no clear damage of ongoing injury (eg hidden infection).
Persistant pain 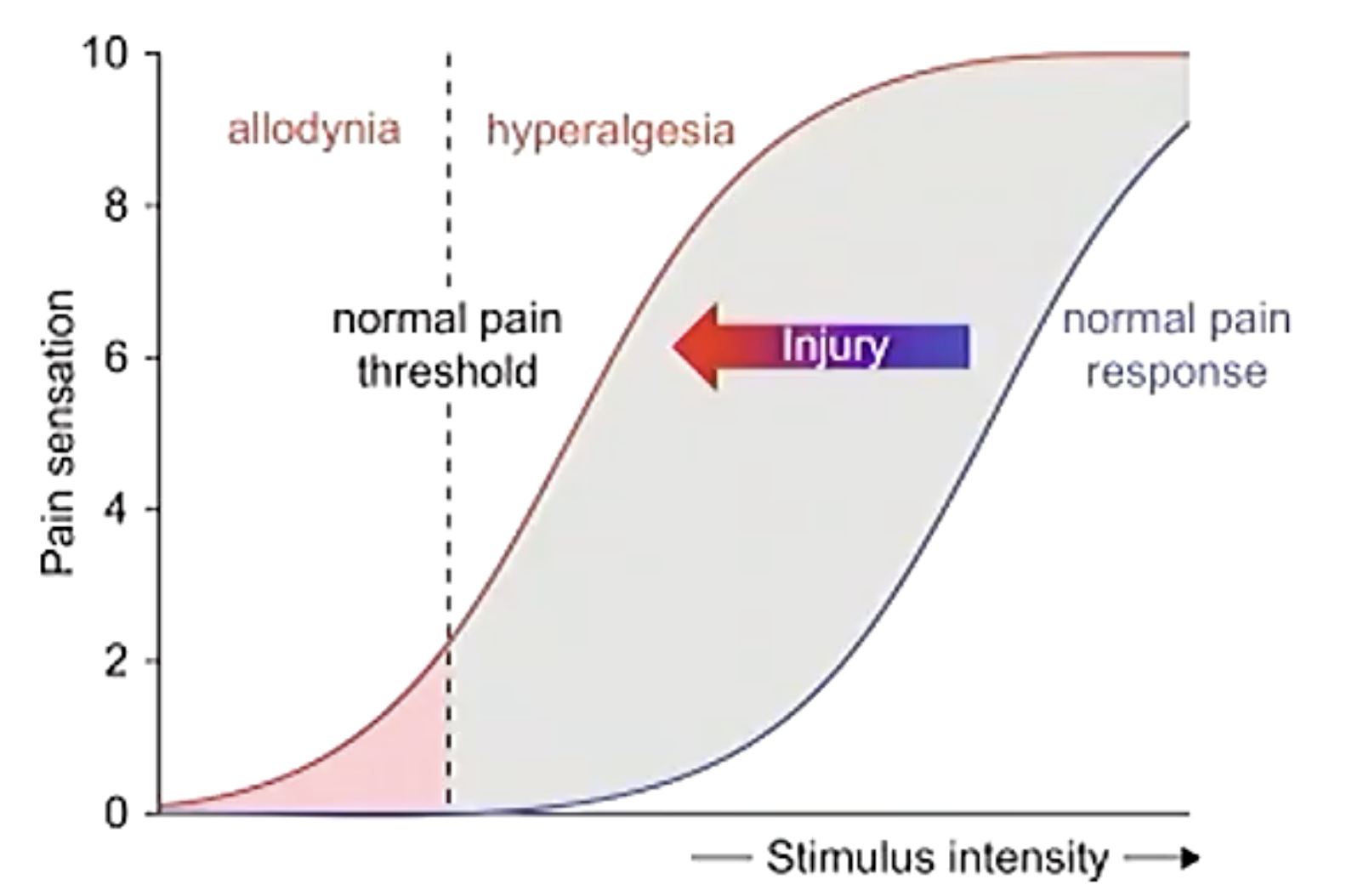
Persistent pain is the result of repeated and ongoing noxious stimulation. It can enhance the sensitivity of pain as well as lead to neuroplastic changes.
Its like the nociceptive signals happen so often that it strengthens the pathway and makes baseline pulses register as nociception
Subjectivity of pain
As pain is an emotional and mental experience many factors affect the experience of pain. for example
- The source of injury
If it is an accident or self inflicted, abuse or treatment, this can affect the feelings of pain.
- Beliefs/concerns
No pain, no gain, if you go to the gym and feel your muscles are sore afterward you don’t have such a negative mindset about it (less applicable example of persistent pain)
- Cultural issues
Language, expectations, expressions health inequity
- Other illnesses and body sensitivity
- Coping strategies
- Social factors
Family, work etc
- Psychological factors
Anxiety and anger, etc
Biopsychosocial perspective of pain (important) 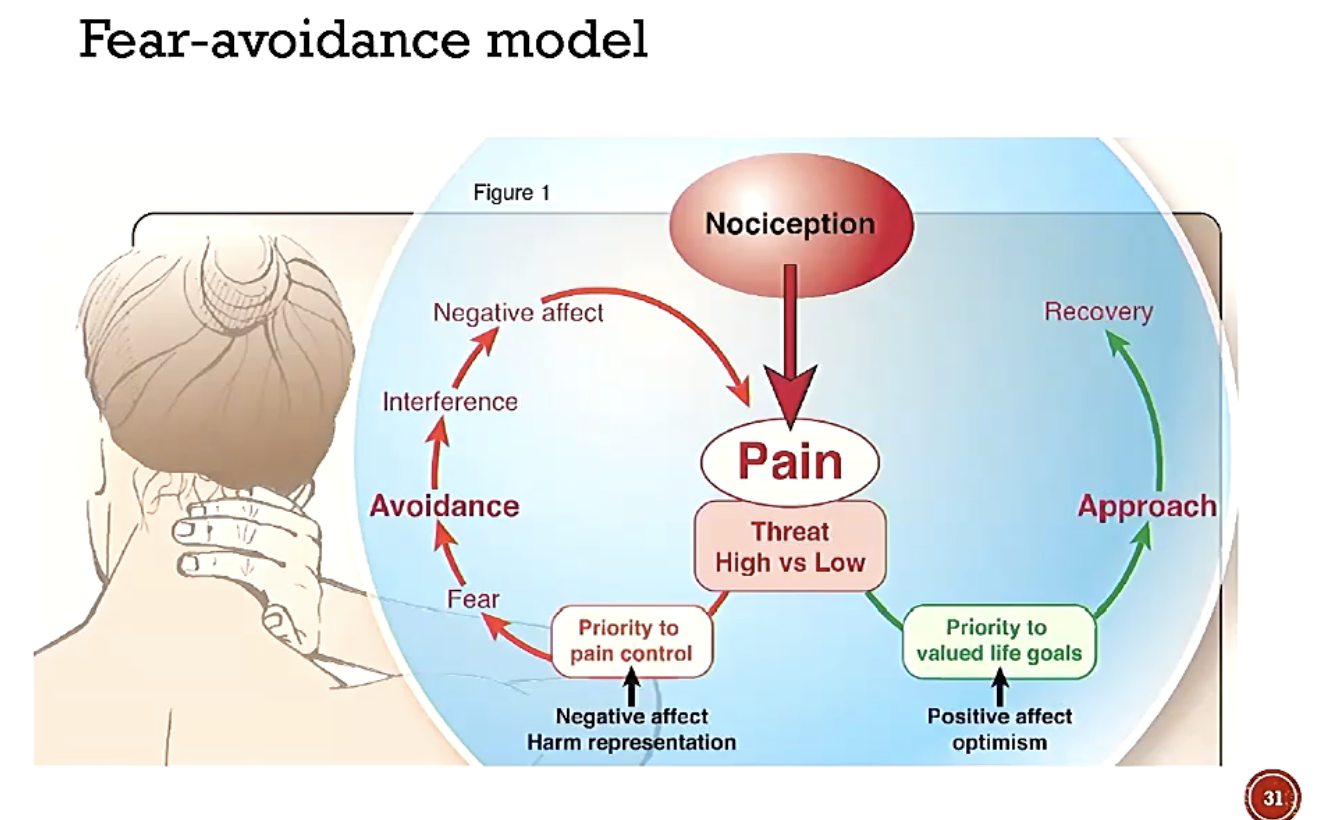
This is a framework to understand attitudes to pain and resulting effects
There are 2 cycles:
Pain control focus
This is where you have a negative mindset about the pain (I’m going to hurt, I’m not going to get better, I cannot manage). This leads to high threat and you focus on the pain, your worry and your body. This leads to fear, and you are always thinking about the pain. You avoid activities that may help you or make you feel better, or push through and injure yourself more. It interferes with your life and as it does it negatively affects you, leading to further high threat thoughts
Focus on life
Optimistic focus leads to more pain reduction.
Clinical approach to pain
Pain management
These people are involved with helping
- Physician
- Occupational therapist
- Nurse
- Physical therapist
- Psychologist
Working with patients with pain
- Build support, use active listening, validate and normalise
- Find out more about the pain (clinical skills connect)
- frequency, intesity, duration of pain
- Area of pain or injury
- Description of pain
- What makes it better and worse
- Impact of pain
- as well as assessing the other factors of the subjectivity of pain
Footer
Relevant lectures: L2 Psych med Other links in medwiki: Comments: