As we have seen with the past lectures breathing needs to be tightly controlled for the purpose of maintaining oxygen levels and blood pH despite changing physiological demands (eg exercise) This is done in a system with 3 main yet interconnected components:
Central control of breathing 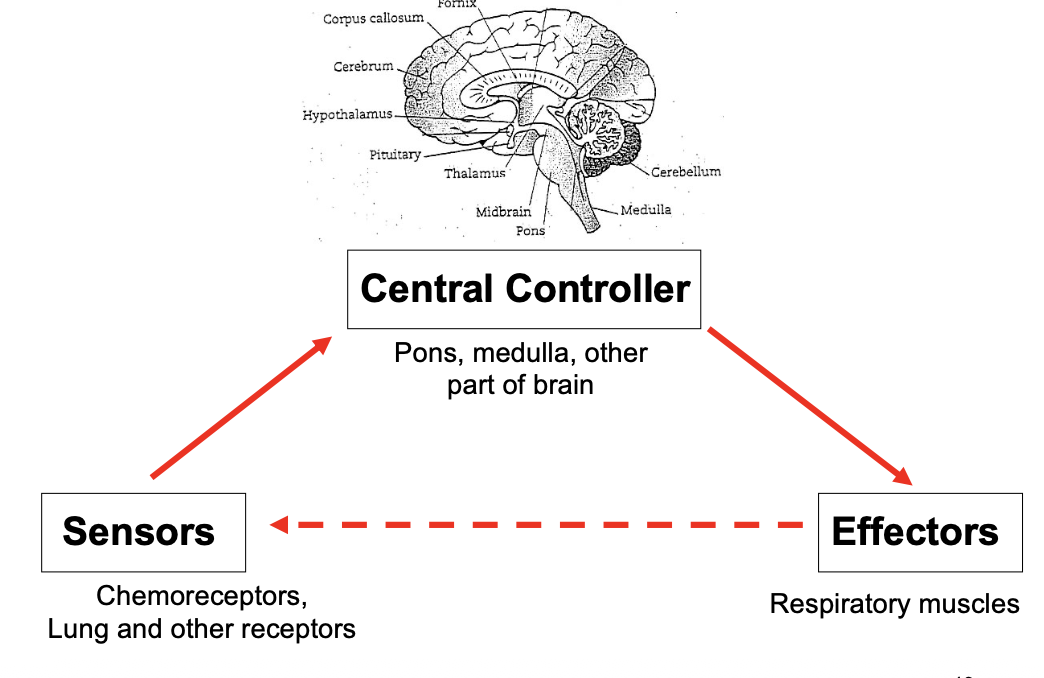
- Central control in the brainstem (respiratory centre)
- This sets rhythm and pattern coordinating the sensors with the effectors to maintain respiratory homeostasis
- Sensors central and peripheral
- This gathers information (chemical and physical)
- Effectors respiratory muscles
- This adjusts actual ventilation
Central controller
The normal automatic processes of breathing stem from the brainstem. the cortex however can override this for voluntary control. The respiratory centre receives a great number of neural and chemical input from both the peripheral and central receptors.
Specific regions of the respiratory centre 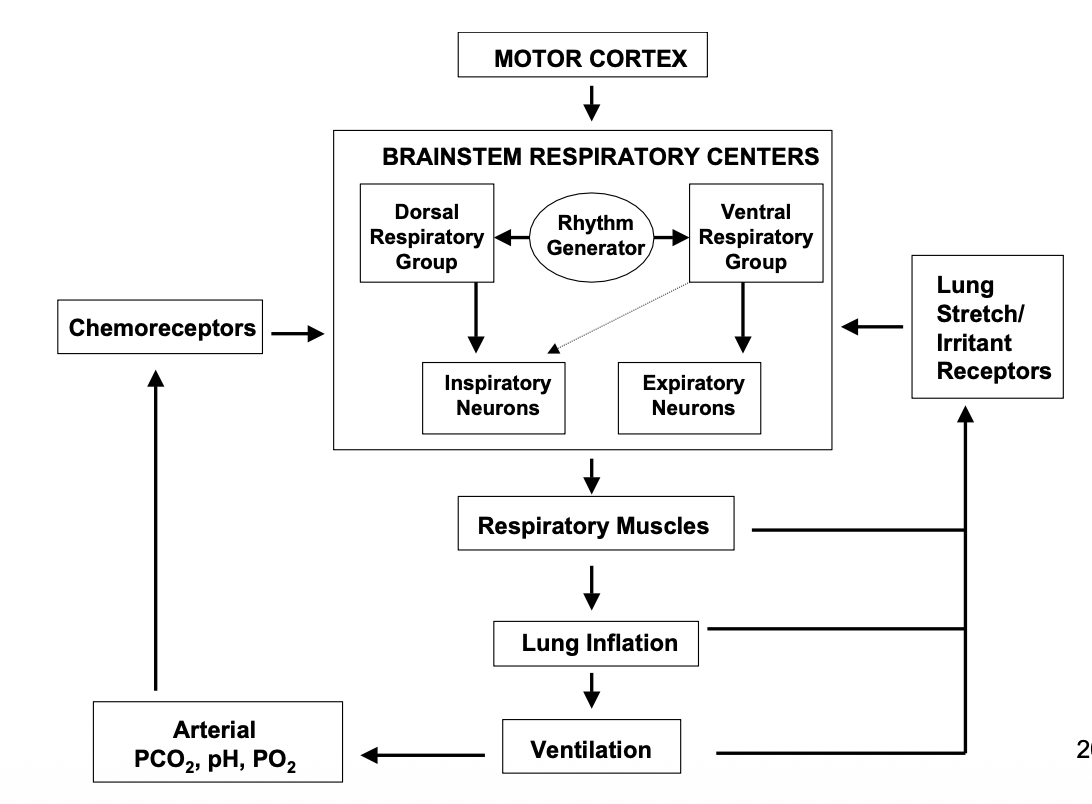
- medullary respiratory centre
- Pre-botzinger complex - rhythm generator / pacemaker
- Dorsal area respiratory group - inspiration
-
Ventral area respiratory group - expiration
- apneustic centre - pons - inspiratory cut off?
- pneumotaxic centre - pons - finetuning? The major output is the phrenic nerves
Sensors
There are central and peripheral sensors.
CCRs
The central chemoreceptors are located near the ventral surface of the medulla and is sensitive to the PCO2 of the blood but not the PO2. This is due to mechanism of sensing the PCO2. The CCRs respond to changes in pH of the ECF/CSF which matches the Blood as CO2 diffuses into the CSF.
PCRs
Located in the carotid and aortic arteries. These guys respond to decreases arterial PO2, increased PCO2 and H+. Due to the fact they response to everything they are responsible for >90% of O2 response and ~20-30% of the CO2. They rapidly respond to changes in blood oxygen and pH levels.
Ventilatory response
to CO2 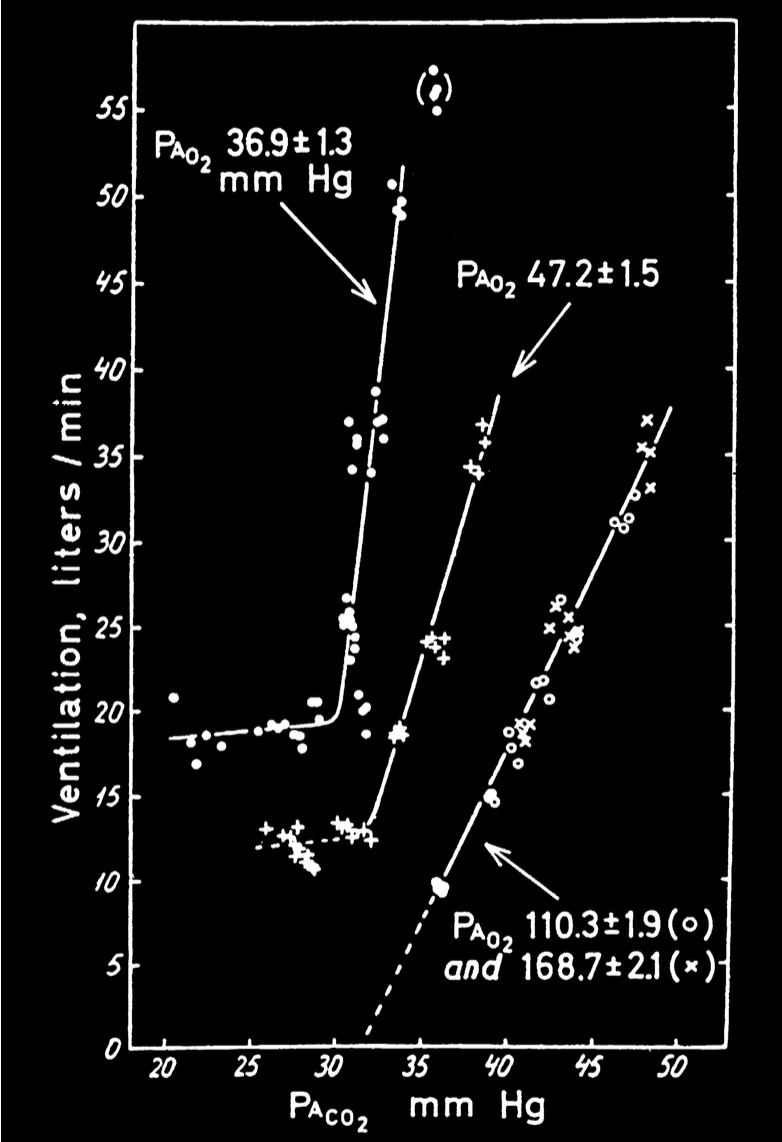
PaCO2 is the most important stimulus to ventilation. It is tightly controlled to within +/-3mmHg of normal.. Most of the stimulus comes from CCRs but PCRs contribute too and their response time is much faster.
Ventilatory response to PCO2 is lessened by sleep increasing age and genetic factors but heightened by low O2. This is displayed nicely in the graph to the right.
to hypoxia
The response to hypoxia is only initated by the peripheral chemorecptors which have little activation during normoxia, but has their response augumented by Hypercapnia. This ensures ventilation is stimulated at Pa02 levels above 60 mmHg.
When PaO2 becomes the primary drive of ventilation.
Hypoxic control becomes dominant in high altitude condition and chronic hypercapnia caused by chronic lung conditions aka CO2 retainers.
Chronic hypoventilation (chronic emphysema/bronchitis) leads to CO2 retention. this leads to high PCO2 and higher HCO3 retention which levels out blood acidity which maintaining that high levels of PaCO2. The capnic response in the CCRs are dulled due to normal pH. Now these people will not feel the need to breathe until hypoxic. Hypoxia is now the main drive of ventilation. This has Important ramifications which I will detail shortly.
In summary: hypoventilation due to increased work of breathing, diffusion problems and/or V/Q mismatch makes patients hypoxic which can become the main drive of ventilation.
Ramification: What if we administer high O2 mix?
more O2 means hypoxia is reduced (and therefore ventilatory drive) and patients will build up massive amounts of PaCO2 in blood.
Nonchemical control of breathing
Other receptors which influence breathing are the:
- Lung receptors
- Slowly adapting stretch receptors
- Rapidly adapting stretch receptors
- Juxtacapillary receptors ( question )
- other receptors
- Nose/airway receptors, joint muscle receptors, arterial baroreceptors, pain and temperature.