- Describe the pathological features of primary pulmonary TB – namely, the ‘Ghon Complex’; and list the possible outcomes following primary infection, including ‘miliary’ TB
- Describe the pathogenesis and pathological features of secondary/reactivation/reinfection pulmonary TB
- Describe the pathogenesis and morphology of extra-pulmonary or isolated-organ tuberculosis
- Describe the principles of diagnosis and treatment of tuberculosis
Mycobacterium tuberculosis
This is an aerobic bacillus which has a capsule. The bacteria is called an acid-fast bacilli because they resist decolorisation by acid in a gram stain so cannot be gram stained. A stain called the Ziehl-Neelsan stain is however able to visualise them.
PCR is the best way to visualise them
Transmission
M. tuberculosis is primarily transmitted through airborne particles (droplet infection), These are generated when an infectious person caughs sneezes talks really anything,
People with extrapulmonary TB or latent infection are both not infectious. Upon exposure to the organism ~30% of people become infected and but only 5-10 % develop disease. Infection is distinct from disease
Intestinal and oropharyngeal tuberculosis is caused by mycobacterium bovis and is contracted through drinking unpasteurised milk from infected cows. BCG vaccine (currently used vaccine) uses attenuated M. bovis.
Immune response to M. tuberculosis infection
Infection
This is the timeline of infection (roughly)
- The inhaled M. tuberculosis organisms (in a naive host) travel deep into rhe lung tissue and get phagocytosed
- Inside the macrophage they resist the phagolysosomes (through a number of virulence factors) and proliferate.
- Proliferation withing the pulmonary alveolar macrophages and air spaces result in bacteraemia and seeding of multiple organs during primary infection,
- Most people dont feel anything yet though
Response
- about 3 weeks after infection the T cell mediated response begins, as the M. tuberculosis antigens have entered the hilar lymph nodes and have been presented to T-cells, which then differentiate into Th1 cells
- The Th1 cells produce IFN-γ which enhances their bactericidal power
- Active macrophages secrete TNF which increases monocyte and macrophage recruitment
- the activated macrophages are now called Epithelioid cells. These epithelioid cells, along with monocytes and lymphocytes cone together to form TB granulomas
- Central caseous necrosis
Granulomas 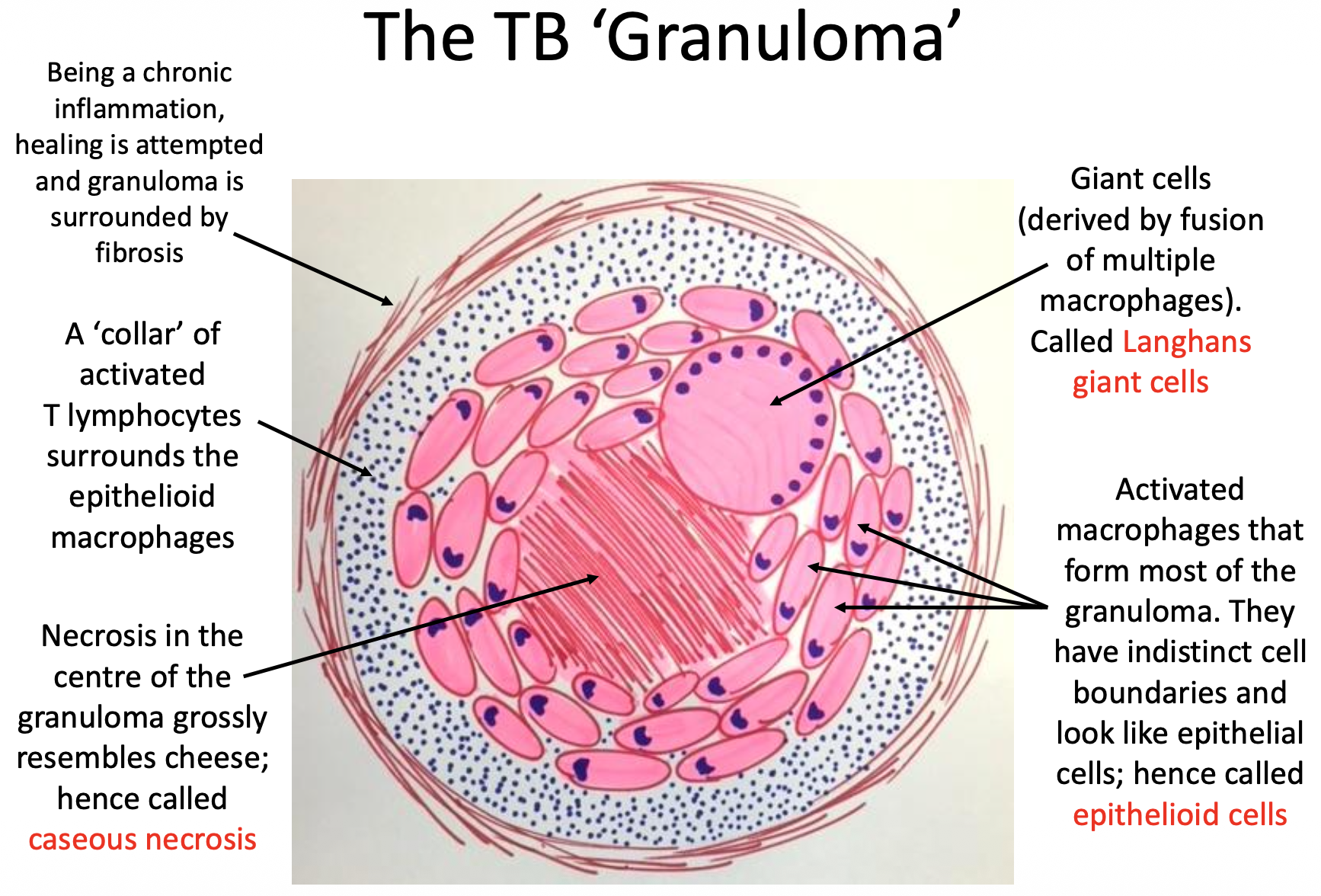
These are little “jails” to contain colonies of M. tuberculosis. they are roughly spherical with a centre of caseous necrosis surrounded by epithelioid cells (activated macrophages). These epithelioid cells are surrounded by sensitised T lymphycytes. occasionally the macrophages can merge into a larger Langerhans giant cell.
This is a hallmark feature of TB and can be found in any tissue where TB can grow
Granulomatous Inflammation
This type of inflammation is a specific type of chronic inflammation which can be present in several diseases and can also happen to foreign bodies. They are the result of persistent activation of T cell-mediated response by a hard to eradicate organism. It is also classified as type 4 sensitivity, TB is always characterised by granuloma
Primary pulmonary TB
Primary TB is the first infection from TB. The terms Ghon focus and Ghon complex describe the lesions from TB, with Ghon focus referring the first point of infection from TB (often also the most progressed, as has been there the longest), and the Ghon complex refers to the Ghon focus and the hilar lymph nodes which also develop granulation and caseation, (I really struggle to understand the significance of this. I guess it brings attention to how this disease evolves over time but really its just the infection in the lung and lymph nodes)
Possible outcomes
After primary infection there are a few outcomes that can happen.
- Eradication of disease (~90%) This is where you win over TB. The infection is halted and the bacteria are killed. the ghon complex is healed via fibrosis and often calcifies, which you can see on X-Ray.
- Latent disease This is a stalemate between the body and the bacteria. The bacteria remains dormant inside the focus of infection in the lung or at other sites in the body. It is waiting to be reactivated if the hosts immunity drops.
- Progressive Primary TB (and sometimes miliary TB) In these cases the infection progresses further, leading to ongoing necrosis and lung tissue damage, You may also have Miliary TB as part of this where there is haematogenous spread of the M. tuberculosis organisms and so granulomas form all over the body, like millet seeds
Secondary pulmonary TB (Chronic Fibro-caseous TB)
This is where there is reactivation of latent disease or reinfection, The immune system already has been sensitised to M. tuberculosis and exhibits an extreme and destructive immune reaction against the organism. This leads to multiple confluent large granulomas with extensive tissue necrosis, surrounded be fibrosis. Secondary lesions often form in the apical parts of the lung (m. tuberculosis is aerobic)
Pathological features
Cavities
As your lung tissues necrose into caseous matter you start to cough it up, leading to holes in the lung. (these are disgusting to be honest and very gross)
Extrapulmonary/isolated organ TB
The haematogenous spread of TB can seed other organs and these extrapulmonary granulomas can become reactivated, sometimes independantly of lung symptoms. This is isolated organ TB and can affect a localised area with chronic infection and necrosis without great symptoms until its too late.
Diagnosis and treatment
Diagnosis
Definitive Diagnosis is made by isolation of the organisms from a sputum sample or from tissue samples from an infected extra pulmonary site using PCR or Zeihl-Neelsen stain. Found granulomas are very suggestive of TB but arent definitive. You can also do a chest X-ray, Mantoux test or interferon gamma release assay.
Possible clinical presentation of active TB
- Cough
- Sputum
- Haemoptysis
- Night fever and sweats
- or other symptoms of Extrapulmonary TB
Mantoux test (tuberculin skin test, TST)
This is where you intracutaneously inject purtified protein of M. tuberculosis and a positive is a swelling that peaks -48-72 hours after. A positive indicated current infection (latent or active).
False negatives can occur with certain viral infections, malnutrition or immunosupression. False positives can reult from prior BCG vaccination.
Interferon gamma release assay
Th1 cells from someone with immune reactivity to TB will release Interferon-γ when exposed to m. tuberculosis antigens which is measured. This is less likely to give false positives or negatives and so is preferred to TST.
Treatment
Multi drug therapy is recommended to combat drug resistance and because certain drugs work for intracellular organisms and certian drugs work for extra cellular organisms
There is a 6 month, 2 phase regimen which is:
- Intensive bactericidal phase
- 4 drugs for 2 months: Isoniazid, rifampacin, ethambutol, and pyrazinamide
- Sterilisation phase
- 2 drugs for 4 months: isoniazid, rifampacin
More prolonged treatment is required for extrapulmonary tb and there are Several treatment regimens for latent disease
Second line antibiotics are availible for multidrug resistant TB