Calcium Channel Blockers Nitrates
Calcium channel blockers
need to know how they work, why they work and selecticity
calcium channels
L-type Long lasting important for cardiac and vascular SM abundant in cardiac and vascular smooth muscle
T-Type Neurtons and pacemakers
Calcium Channel blockers
blocks L and T-type channels chemically and pharmacologically heterogenous antagonises calcium passage different binding sites result in tissue selectivity alpha subunit varies
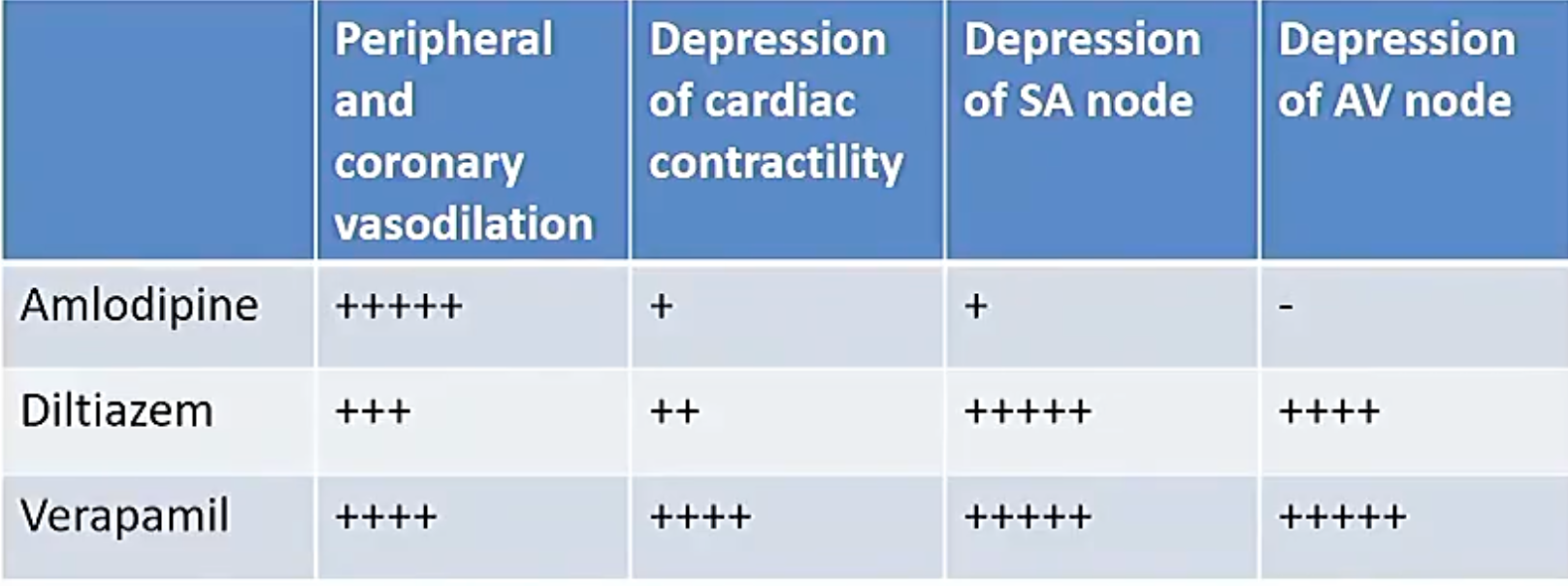
act to: reducing vascular tone reduce cardiac inotrophy reduction in sa node chronotrophy decrease conduction velocity into ventricles (AV node)
atrial block to ventricles (av node)
often reflex tachycardia from really quick drop in BP
How selective are these
MAIN indication for CCBs hypertensions DHP arrhythmias diltiazem angina verapamil diltiazem
advantages doesnt induce bronchconstricition doesnt induce poor lipid profiles
Dihydropyridines (vasoselective) (‘dipine)
amlodipine MOA binds to and inhibits l- and T- type channels antihypertensice due to vasodilatory acts more on arterial smooth muscle amlodipine reduced afterload and cardiac O2 consumption little effect on preload due to most venous beds being fine
Amlodipine binds to inactivated L-Type Ca channels and stablises them as inactive inactive channels are more likely to be found in arterial sms as depolarisations are longer lasting
beware in angina due to reflex tachycardia some dihydropyridines are associated with oedema
completely absorbed from GI tract slow onset steady state in around a week extensively hepatically metabolised and excreted into urine as inactive metabolites
only 10% excreted unchanged in urine
Phenylalkylamines (cardioselective)
verapamil
bind directly to open cardiac L-type channels therefore relatively cardioselective
suppresses cardiac contractility reducing cardiac work
also acts as vasodilator with selectivity for arterial vasculature
usually withough reflex TC
MOA binds to open state and promotes inactivated channel conformation as well as slows channel recovery from inactivation
higher rates of channel inhibition
Indications angina
- reduced cardiac o2 demand
- reversess coronary vasospasm hypertension
- antihypertensive
contraindications avoid in heart failure comcommitant use with b blockers can induce heart stop
however in bradycardia or conduction defects it can just stop the heart via heart block
PK rapid and near complete oral absorption exrtensive 1st pass can increase plasma conc in poor liver patients
IV route is good for avoiding liver
Benzothiazipines (cardioselective)
diltiazem
MOA
inhibiting Ca2 influs during membrane depolarisation of primarily cardiac and vascular smooth muscle
interferes with cardiac depolarising current in excitable tissue selective mostly for SA and SV node
suitable as an antiarrhythmic heart rate resuced effective as antiarrhythmic in AF
angina
- reduced cardiac o2 demand
- reversess coronary vasospasm
highly absorbed undergoes extensive 1st pass metabloims
lots of drug interactions associated with CYP3A4
General ADR to CCBs extension od drug action hypotension bradycardia AV block HF
caustion iwth other drugs causes cardiac depression if used with BBlockers
What does NO do
Endothelial NO functions include relaxing vascular smooth uscels inhibiting platelet aggregation (useful) inhibiting leukocyte endothelial interactions
Many vasodilators work through no bradykinin acetylcholine histamine etc
- NO is made from L-arginine through eNOS
ach brady kinin ANP and kistamine causes ca to enter cell causing eNOS to activati
chews through arginine makes no and citrulline
no activates guantl cyclase which makes cGMP which promote relaxation cGMP reduces calcium intracellularly
cGMP terminated by phophodiesterase (PDE 5)
Drugs
Nitrodilators mimic NO
Sodium nitroprusside spontanously decays into NO
organic nitrates are ezymatically broken to produce NO intracellularly
coronary arteries arent dilated
main function is to reduce preload
nitrates reduce wall stress and reduce preload and afterload
GTN
can be sublingual spray treatment of acute angine fast acting 2-5 mins
fast halflife and do sublingual is onlo one long enough
isosorbate di/mononitrate
Longer term
Sodium nitroprusside
cerricyanide sponmtanously decays into NO extremely fast acting (aortic dissection (explosion))
tolerance
Tolerance builds
Nitrate adverse effects
Dose related effects flushing headacherelfex tach palpitations ortho hypotension postural dizziness and neusaa have been reported GTN may aggrevate hypoxia by inhibiting hypoxic pulmonary vasoconstriction
high doses of nitroglycerin may produce methaemoglobinaemia nitrites are made from nitrate metabolism which accelerates metHb production
topical nitrates may produce skin reactions
Rebound effects from tolerance preak
drug interactions
PDE5 inhibitors
.