Renal physiology
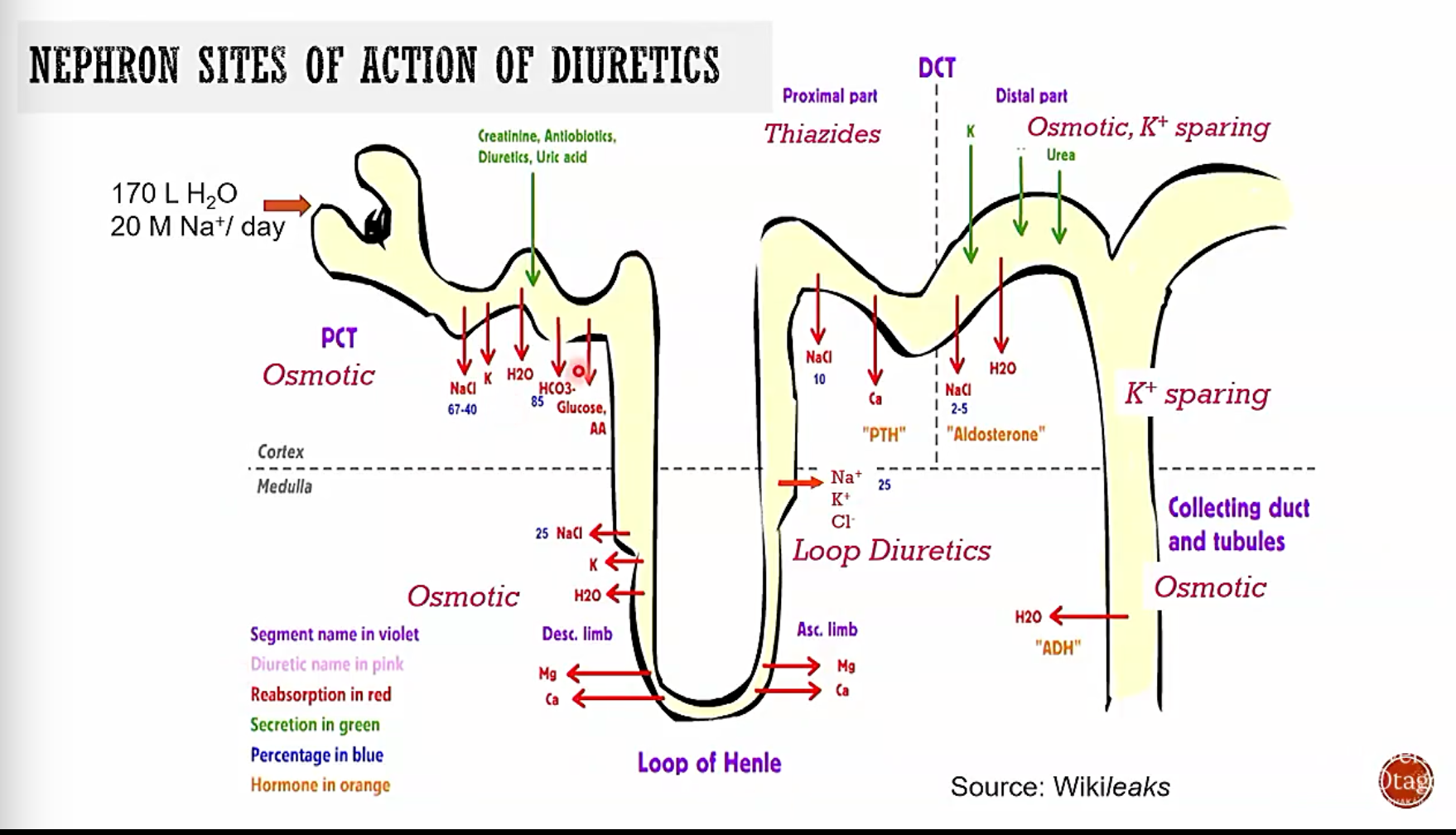
170 litres of water enters tublue per day 20 m of na per day
PCT recovers 60-70% of water and na
PCT also involved in excreting metabolised drugs
basically we can lose great amounts of volume from blood if we change the nephron dynamics
PCT mediates secretion and reabsorption of weak acids and bases through organic anion transporters
NKCC2 has capacity to absorb ~25% of NA+ load Found in TAL
ROMK and basolateral CLC-K2 cause a transmembrane potential to form leading to reabsorption of Na Ca Mg ions
Aldosterone effects
aldosterone is a steroid and gets into cell where it triggers AIP to be made (aldosterone inducible proteins) make k and na+ channels and increase atp generation for more na k atpase
Diuretic mechanisms
mannitol (and other osmotics?) are freely filtered and
Other diuretics are highly bound to proteins
most diuretics are weak acids so use OATS
Drugs
Osmotic diuretics e.g. mannitol
Site of action
Mannitol
given IV as we dont want it to pull lots of water into gut
pharmacologically inert but osmotically active
freely filtered in glomerulus but not really absobed into PCt
hinders water reaborption from tubule
Use
emergency reduction od intercranial pressure (not the best drug for it) it pulls water from cells into ECF and blood can cause pulmonary congestion and can cause dehydrative effects
Other diuretics are highly protein bound
Loop diuretics e.g. frusemide (furosemide)
sledge hammer
Site of action: thick ascending loop
makes people feel like they pee from a high place can be given orally of through IV uses for high levels of volume unloading
Most potent diuretics available chemically diverse range
Inhibit NKCC2 (na k cl cotransporter) competing with Cl- for binding
Loop diuretics limit absorption of Na Ca Mg Cl etc highly potent\
actively secreted by PCt (oat)
35% metabolised by glucuronidation/CYP 450
90% bound to plasma proteins
frusemide has great effects to na ca mg cl h+ and k+ loss
drug interactions due to renal changes
side effect can be hypo kalemia
Theraputic usage of loop diuretics
- HTN
- oedema
- cardiac renal or hepatic origin
- maintaining renal funtion in renal injury
- acute pulomary oedema
- hyperkalaemia
- hypercalcaemia
side effects
hypovolaemia dizziness syncip etc Na+ loss K+ loss ma and ca depletion metabolis alkalosis hyperuricaemia (may progress gout) nkcc1 in the inner ear (hearing loss / ototoxicity) can increase renal toxicity of cephalosporin
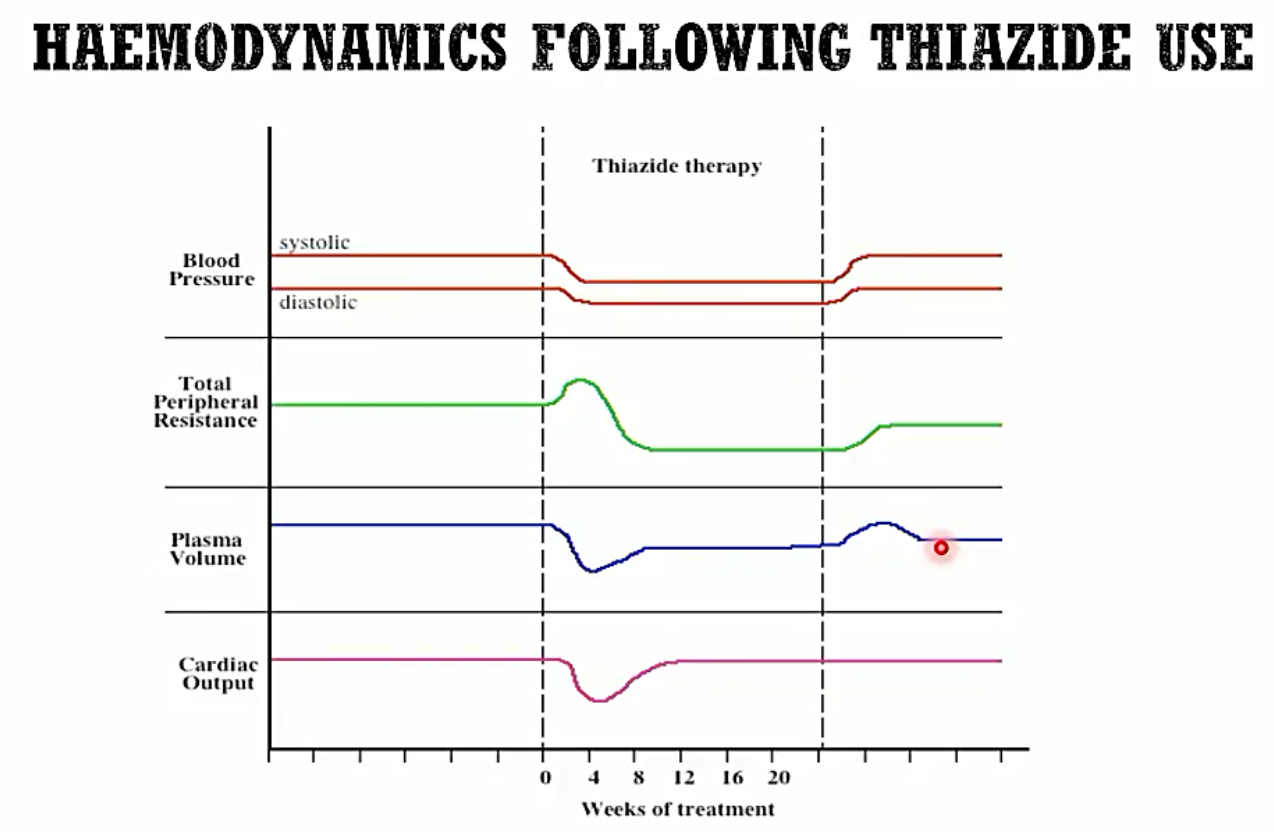
Thiazide diuretics e.g. bendroflumethiazide
moderate diuretic 2nd line therpaty for htn
MOA
competitively bind to apical eNCC-1 (nacl cotransporter) eNCC1 upregulated by aldosterone
excreted by
theraputic usage
oral delivery HTN used with ACEI / ARBS and CCbs monotherapy in elderly HTn if there is little raas conponent can be used in renal disease acute pulmonary HTN
also due to slight hyponatreimia less firing in smooth muscle and cardiac firing etc
Adverse effects
dehydration and postural hypotension electrolyte imbalance hyponatraemia (increased na loss can lead to li+ retention) hypokalemia metabolic alkalosis uric acid retention
K+ loss may induce torsades de pointes
hyperglycaemia
K+ spareing diuretics e.g. spironolactone (amiloride)
minerocorticoid receptor antagonist blocks aldosterone
just acts on the basolateral side
toxicity increase potassium retention androgen modulating effects (Reduced testosterone effects) gynocomastera