Skin infections are often caused by pyogenic gram-positive cocci, most common of these are Staphylococcus aureus and Streptococcus Pyogenes.
Pyogenic?
Pyogenic means pus producing (synonyms are purulent, or suppurative) and pus in this case specifically refers substance composed of bacteria (dead and alive), neutrophils, and fibrin rich inflammatory exudate. often this is within an abscess (of varying size) caused by the infection.
Other key concepts…
Some commensal bacteria can be opportunistic and when given the opportunity will try to infect you, the presentation of the infection is related to both the site of infection as well as the characteristic of pathogen and host.
NZ has high rates of skin infection compared to similar countries.
Major actors
The 2 big pathogens causing this are Staphylococcus and streptococcus These are similar but can be differentiated on gram staining
Types of infection
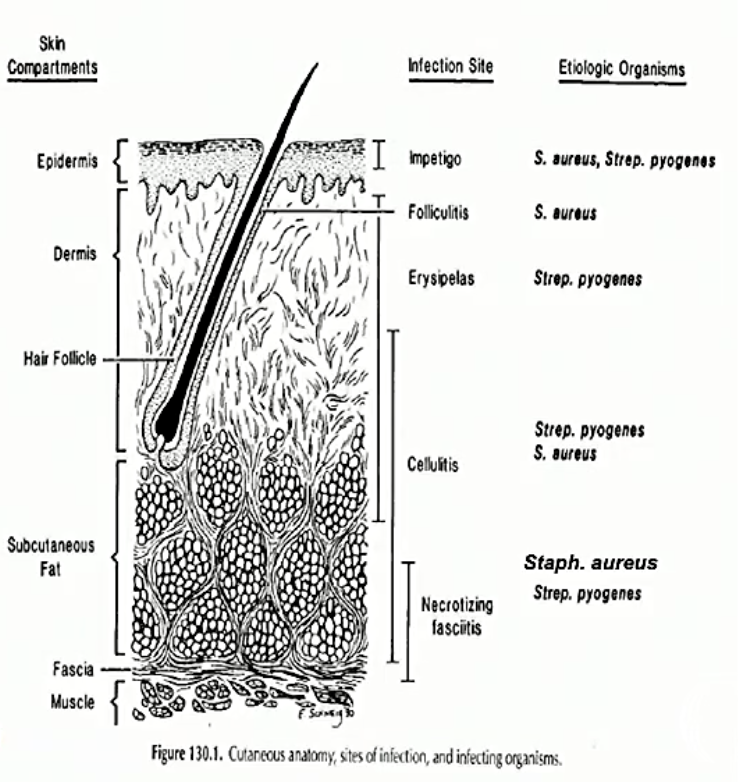
these are the types of pyogenic skin infections you can get. The most mild (and superficial) at the top and the most serious at the bottom (also the deepest).
Pyodermas
Impetigo
This can be bullous (with blisters) or non-bullous (without blisters).
- Non-bullous can be caused by S. aureus and or S. pyogenes. It mostly infects children around the mouth. It often looks like thin walled vesicles (little blisters) which lyse (pop) to form honey coloured crusts/thin scabs.
- Bullous is only caused S. aureus and means it is producing a very specific toxin, an epidermolytic exotoxin (exotoxin meaning the toxin is secreted) (this breaks down desmosomes). It is characterised by large fluid filled vesicles. may occur anywhere and affects all ages.
- Diagnosis is based on clinical presentation.
Folliculitis
- Infection of Hair follicles. Starts out looking like small papules (little red bumps) and evolves into pustules (little pimple looking things). This is a superficial infection.
- It is usually caused by S. aureus usually means coagulase and adhesins are present. You can culture the pus.
- It tends to be selflimiting and consider topical antiseptics and wound care. Dont consider oral antimcrobial if there is extensive disease, topical treatment fails, or infection progresses.
Furuncles (Boil)
- This is a larger boil which can often arise from a progressed folliculitis. It is a deeper infection of the hair follicles. Still really S. aureus containing coagulase and adhesins. Complications include abscesses and cellulitis.
- You probably need risk factors for this to occur which are:
- Diabetes
- Obesity
- S. aureus carriage
- and immunosuppression
- Treatment consists of surgical drainage and oral/IV antimicrobials
Carbuncles
- Progression of Furuncle. Really just a extensive cluster infection of follicles, and usually effects The neck back and thighs, Usually caused by S. aureus (PVL+ and coagulase).
- The risk factors for this to occur are:
- Older age
- Diabetes
- Prolonged steroid therapy
- Clinical presentation: The presentation Is a hard painful lump with suppuration (pus formation) after 5-7 days. Necrosis can lead to an ulcer as well,
- Diagnosis
- You can culture the pus and look for antimicrobial sensetivities
- Treatment
- Surgical drainage and oral/IV antimicrobials
Cellulitis (not cellulite)
- This is a spreading infection in the skin involving deeper layers such as the dermis or hypodermis. Can be small (redness around acne) or large (entire limb).
- The symptoms present as oedema with little to no necrosis, ill defined margins which smoothly blends to normal skin. Pain, heat, swelling and erythema (redness) can present, along with fever, chills, nauseam and leukocytosis.
- In 30% of cases there is bacteraemia.
- ComplicationsL
- abscess, osteomyelitits, septic arthritis, sepsis, Necrotising fasciitis
- Most commonly caused by S. aureus. and S. pyogenes. Can be polymicrobial though
- Risk factors that can cause this are bascially anything which can decrease immunity or break defenses
- Diagnosis: often you can do a clinical diagnosis and try to culture aspirates, abscesses, pustules or wounds to assess antimicrobial sensitivities.
- Treatment depends on extent of infection host status, and causative agent. If in concern begin empiric treatment
Erysipelas
- This is a cellulitis exclusively caused by S. pyogenes (with invasins) and it is a superficial cellulitis with lymphatic involvement,
- Symptoms include bright red well differentiated swelled lesion, systemic symptoms include fever chills malaise adn leukocytosis, it typically affects the face or legs
- Risk factors: this often occurs in elderly, children and infants. Anything which causes immune deficiency is a risk factor
- complications and treatment is the same as cellulitis
Necrotising fasciitis (gross as hell
Both Cellulitis and Necrotising fasciitis can be gram negative or a polymicrobial infection
- Necrotising fasciitis is like cellulitis on meth. It is a rapid, spreading, destructive infection along fascia
- High mortality
-
90% if treatment is delayed or not given
- ~20% even with aggressive therapy
- Causes sepsis with multi-organ failures
-
- S. pyogene or S. aureus
- trauma to skin, the wound is often small. Tissue destroying virulence factors are important for this to occur.
- risk factors are anything that decreases immunity
- Diagnosis
- Clinical mostly
- Laboratory finishthis
Treatments
Pyodermas
For minor infections avoid antimicrobials and use wound care and topical antiseptics. Maybe topical antimicrobials Use oral antimicrobials if there are risks, lack of response or progression.
Abscesses
Surgical drainage and maybe oral/IV antimicrobials
Cellulitis
High risk for complication in high risk patients. use oral/IV antibiotics in this case and empiric therapy if its serious
Necrotising fasciitis
IV antibiotics (initially empiric) and surgical debridement (even amputation)
S. aureus
more than 50% penicillin resistant so use flucloxacillin If MRSA use vancomycin
S. pyogenes
Use penicilliin or macrolides in penicillin allergy