Link to glossary: Glossary Symbols of Respiratory Physiology
Gas exchange
Lecture denotes how generally a patient will consume O₂ at a rate of 250-300 ml/min and produce CO₂ at a rate of 200-250ml/min. However this needs to be able to be increased in exercise.
Components of alveolar diffusion
Additionally a constant called the Respiratory Exchange Ratio (R) = 0.8 = 200/250. So for every 1ml of oxygen we inhale we exhale 0.8ml CO2 this is due to making water and that carbs supply their own oxygen etc
PAO2 and PACO2 are half of alveolar diffusion a.k.a. it sets the alveolar end. The other is arterial gas pressures.
We cannot measure alveolar gas composition so we must calculate it using the composition of inspired air (PI, alveolar ventilation, O2 consumption and CO2 production, and V=Q. Oxygen is like a balancing game between VA, PIO2 coming in and VO2 going into blood. Carbon dioxide is a balancing game of VA, PICO2 going out and VCO2 coming in
Oxygen
Carbon dioxide
N.B. PICO2 is 0 The alveolar gas equation is thus:
and the ∆A-a as a determinant of decreased diffusion. is it is more than 10 it means there is less gas exchange
and additionally the only things are introducing in this equation (at room air ventilation) is PaO2 and PaCO2. therefore you can figure it all out from this if you just input blood gasses (if they are breathing room air at the right pressure)
Problems with gas exchange
When we don’t get enough loading of 02 into blood (high ∆A-a) this is usually due to 3 main(ish) causes:
1. Impaired diffusion
The causes of impaired diffusion are per Fick’s law:
- Thickening of the diffusion barrier
- Decrease in the surface area
- Exercise (P/q mismatch?)
- Breathing low O2 mix (not sure about this one either)
Some comments on the diffusion of oxygen:
As per diagram: 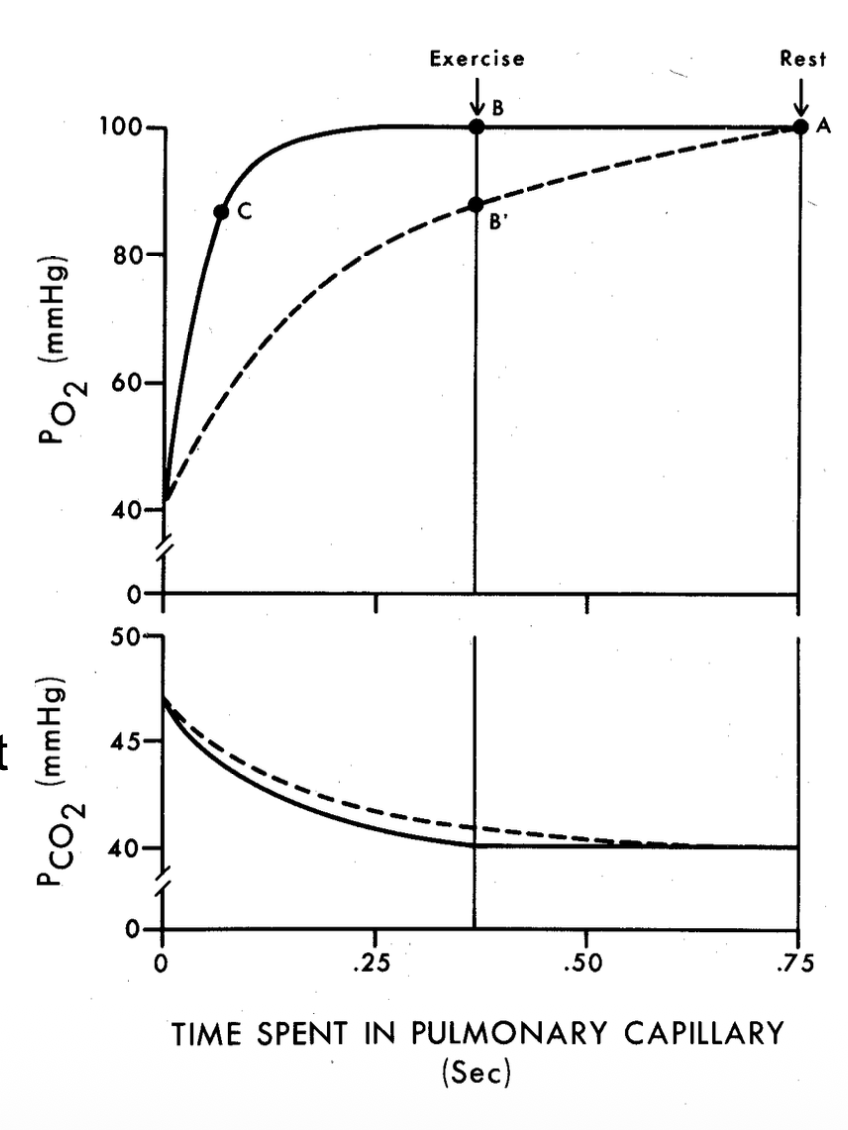 you can see that the time each erythrocyte spends in the pulmonary capillaries is about 0.75 seconds in the pulmonary capillaries. in a healthy individual equilibrium is reached in about 0.25 seconds. You need significant impairment before you get reduced PAO2 at result. However with exercise the time spend in a capillary shortens to 0.25 or so seconds. this can lead to appreciable problems with diffusion. This issue will have good response to extra O2.
you can see that the time each erythrocyte spends in the pulmonary capillaries is about 0.75 seconds in the pulmonary capillaries. in a healthy individual equilibrium is reached in about 0.25 seconds. You need significant impairment before you get reduced PAO2 at result. However with exercise the time spend in a capillary shortens to 0.25 or so seconds. this can lead to appreciable problems with diffusion. This issue will have good response to extra O2.
CO2 diffusion is rarely impaired. its diffusion constant is 23x that of oxygen.
2. Shunt
this is where blood reenters the pulmonary venous drainage without being reoxygenated, diluting oxygenation of the other blood. this may be anatomical, blood being directed to areas what just aren’t full of exchange surfaces, or it could be pathological, eg pneumonia where alveoli are filled with pus. shunts respond poorly to additional oxygen.
3. Ventilation-diffusion mismatch recomplete with watching lecture
this is where the perfusion of blood and the ventilation of the alveoli are not matched for best diffusion. either blood is perfusion at too high a rate for the ventilation which results in blood leaving not having full oxygenation/ full decarbonation, or ventilation is wasted on slow moving blood. in the case of fast blood extra o2 is beneficial
Arterial hypoxaemia
can be caused by (REMEMBER THIS)
- reduced PB or FIO2
- hypoventilation
- impaired diffusion
- Shunt
- V/Q mismatch
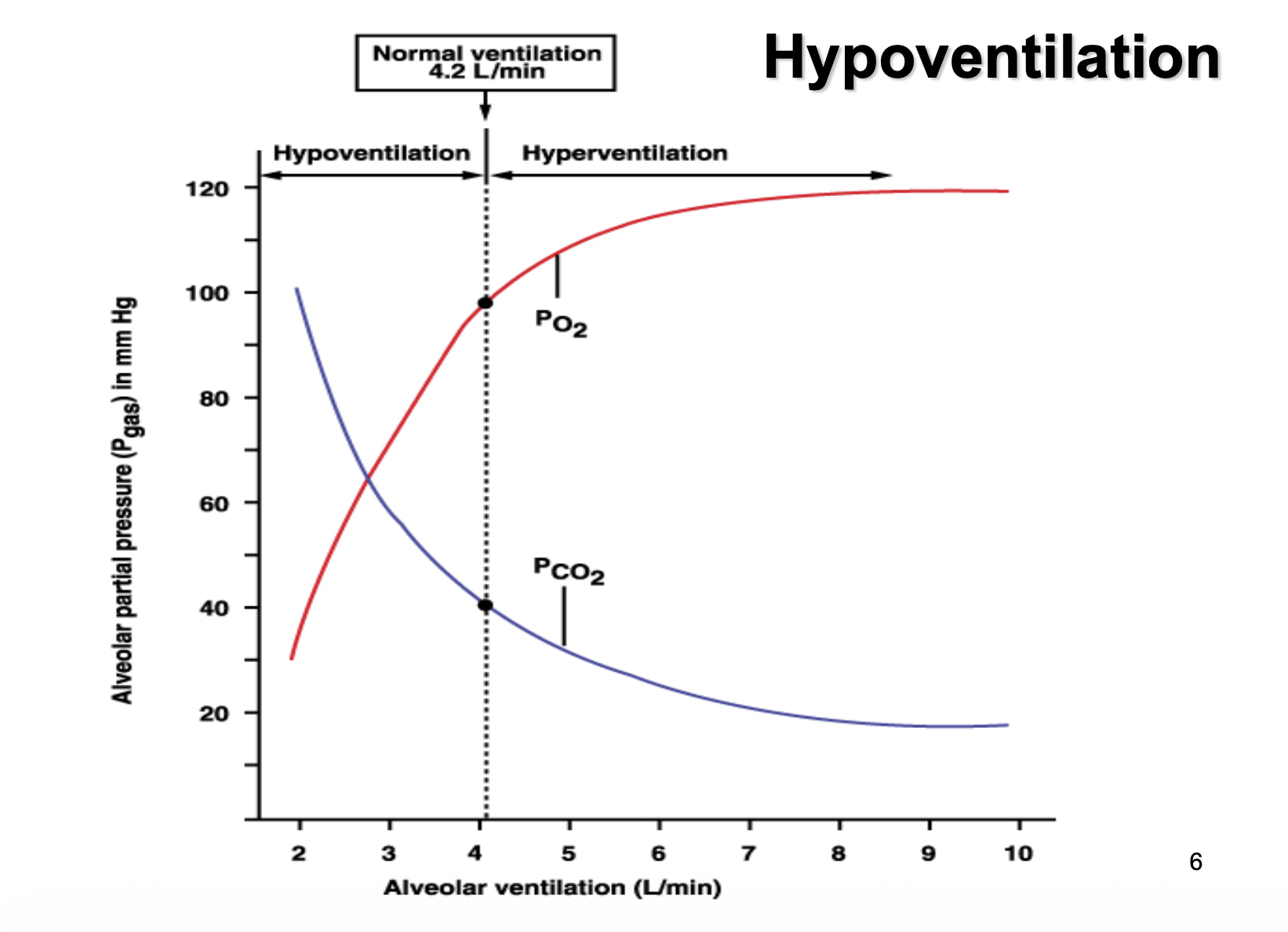
Keeps going about the content in the last lecture. Brings up this neat graph on hypo vs hyperventilation.
Causes of hypoventilation
Hypoventilation
Key properties always increases PaCO2 decreases PaO2 but this is reverible by adding higher concentration oxygen.
Causes:
- high work of breathing
- Damage to chest wall or fatigue
- Respiratory depressants (morphine/barbituates)
- Sleep
Respiratory failure
PaO2 <60 mmHg or PaCO2 >55mmHg Can be type 1 or type 2
Type I PaO2 low PaCO2 normal gas exchagne problems, V/Q dhunt. pneumonia
Type II PaO2 low PaCO2 high ventilatory failure Chronic bronchitis, emphysema